Vaccine Storage: How to Keep Vaccines Safe and Effective
When it comes to vaccine storage, the controlled environment needed to keep vaccines potent from manufacturer to patient. Also known as cold chain management, it’s not just a lab rule—it’s what keeps you and your family protected. A vaccine that’s too hot or too cold doesn’t just lose effectiveness—it can become useless. And that’s not theoretical. In 2022, a clinic in Texas had to discard over 1,200 doses of HPV vaccine because the fridge broke overnight. No one got sick from that, but no one got protected either.
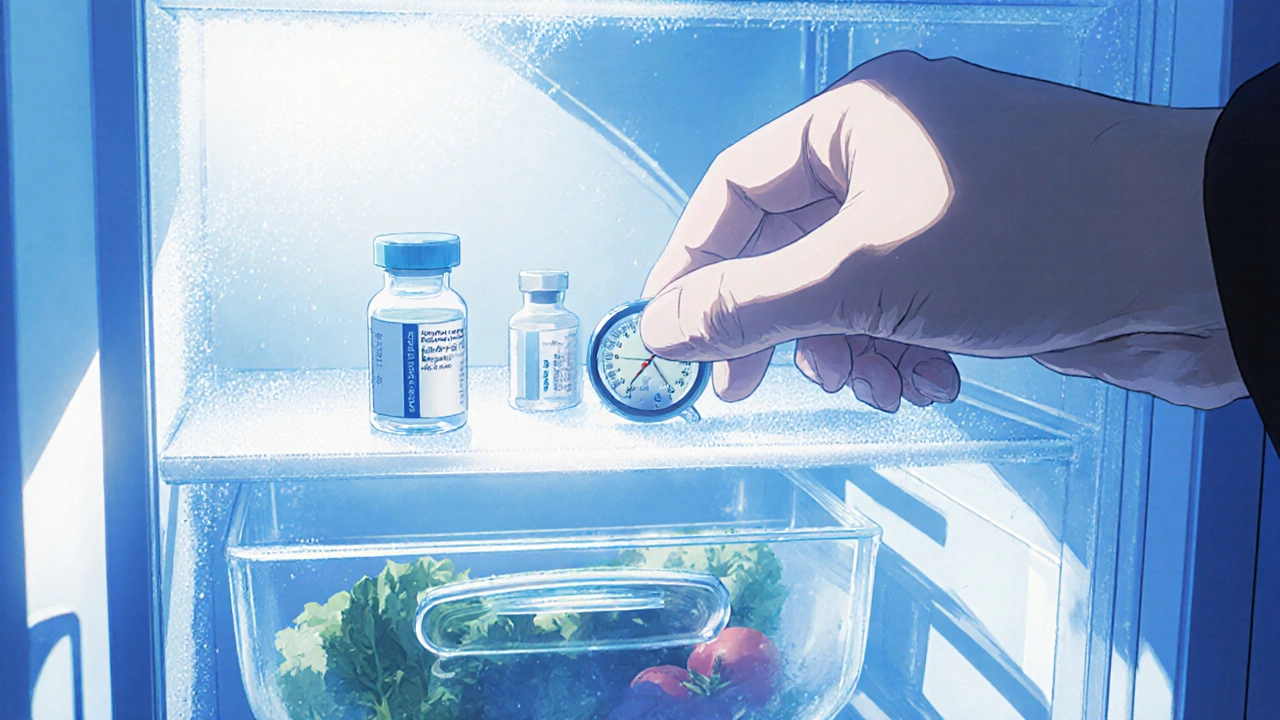
Vaccine temperature, the specific range each vaccine must stay within to remain active, varies by type. Most routine vaccines like MMR or varicella need to stay between 2°C and 8°C. But mRNA vaccines like Pfizer and Moderna started out requiring deep freezing—some as low as -70°C. Even now, after thawing, they can’t sit out for more than a few hours. Then there’s the cold chain, the entire system of storage, transport, and handling that keeps vaccines at safe temperatures. This isn’t just about refrigerators. It includes insulated boxes, temperature loggers, trained staff, and backup power. Break any link in that chain, and the vaccine is at risk.
At home, vaccine storage matters too. If you’re given a vaccine to take home—like some flu shots or travel vaccines—you’ll get instructions. Don’t guess. Don’t put it in the fridge door. That’s the warmest spot. Put it in the back, where the temperature stays steady. Never freeze a vaccine unless the label says to. And if the power goes out, don’t open the fridge. Every time you do, the temperature rises. Keep a thermometer inside. If the temperature goes out of range, call your provider before using it.
Healthcare workers aren’t the only ones who need to get this right. Pharmacies, schools, mobile clinics, and even military field units rely on proper vaccine refrigeration, the practice of using approved units designed to maintain precise, stable temperatures. Regular household fridges aren’t built for this. They cycle too much. They’re opened too often. That’s why clinics use medical-grade units with alarms and digital logs. Even small errors add up. One study found that 25% of vaccine refrigerators in rural clinics didn’t meet temperature standards—enough to compromise thousands of doses over time.
What you’ll find in this collection are real, practical guides on how to handle vaccines safely—whether you’re traveling with insulin and biologics, storing vaccines during a power outage, or checking if your clinic’s fridge is up to code. You’ll see how temperature spikes ruin doses, how to spot a compromised vaccine, and why some vaccines can’t be mixed or transported without special tools. These aren’t theory pieces. They’re written by people who’ve seen what happens when storage fails.