Why Some Medicines Need the Fridge
Not all medicines are created equal when it comes to storage. While your blood pressure pills or antibiotics can sit safely on your bathroom counter, others-like insulin, certain vaccines, and biologic drugs-need to stay cold. Why? Because heat and freezing can destroy their structure, making them less effective or even dangerous to use. The science is clear: if a medication is labeled for refrigeration, it’s not a suggestion-it’s a requirement.
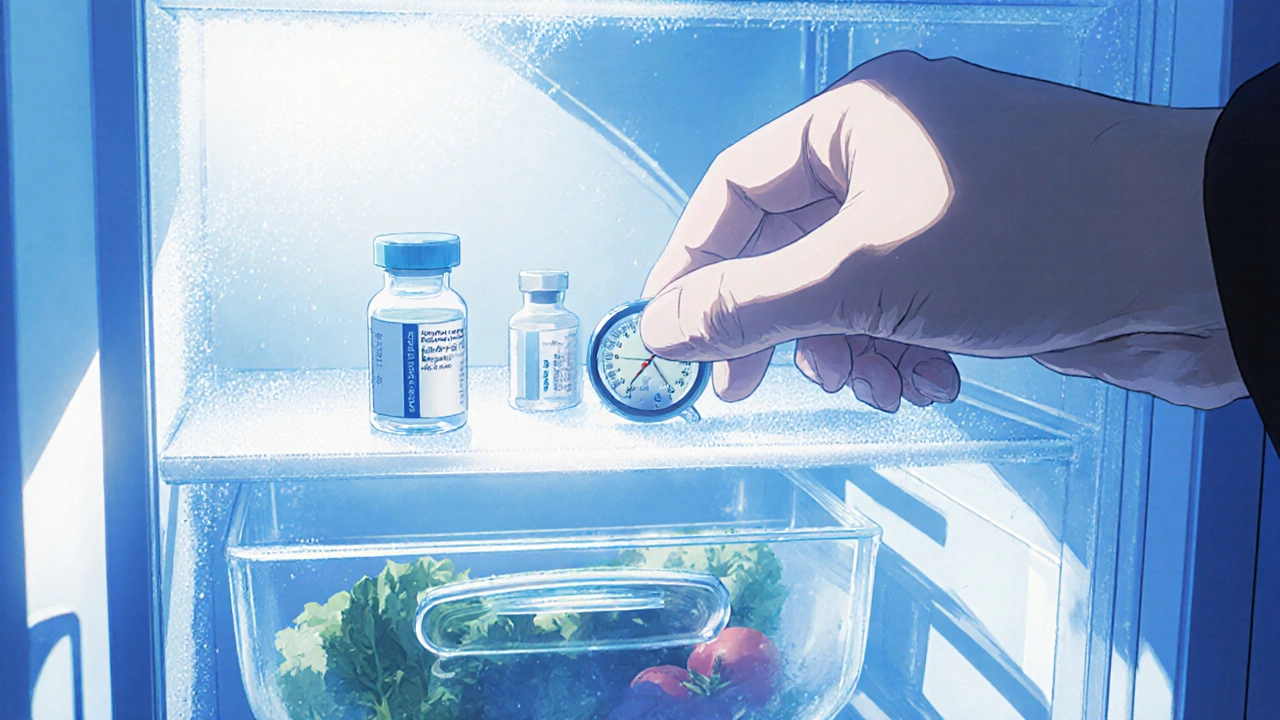
Most refrigerated medications must be kept between 36°F and 46°F (2°C to 8°C). This range keeps proteins stable without freezing them. Freeze a vial of insulin, and you’ve ruined it. Leave it on a sunny windowsill, and it starts breaking down within hours. The FDA and U.S. Pharmacopeia agree: this is the only safe zone for these drugs.
Which Medications Actually Need Refrigeration?
You might be surprised how many common prescriptions require cold storage. Here’s what you’re likely to encounter:
- Insulin (Lantus, Humalog, NovoRapid, etc.) - Must be refrigerated until opened, then can stay at room temperature for up to 28-30 days.
- Vaccines (Flu shots, COVID boosters, MMR, shingles) - Never leave these out. Even a few hours at room temperature can make them useless.
- Biologics - Drugs like Humira, Enbrel, Remicade, and Ocrevus. These are large protein molecules made in labs. They’re fragile. One study showed some lost 50% of their potency after just 24 hours at 77°F.
- Some antibiotics - Like reconstituted amoxicillin clavulanate or certain IV antibiotics. Check the label.
- Eye drops - Certain glaucoma or post-surgery drops, like latanoprost, need refrigeration after opening.
And here’s the catch: just because your doctor gave you a vial that looks like a regular shot doesn’t mean it’s safe to leave on the counter. Always read the label. If it says “store in refrigerator,” don’t guess.
Household Fridges Are Not Designed for Medicines
Your kitchen fridge isn’t built to keep medicine safe. It’s built to keep milk cold and veggies crisp. That means temperature swings are normal-especially near the door, where it can hit 60°F on a busy day. A 2022 study found that the back of the fridge stays steady around 3.4°C, but the door shelf? It averages 11.3°C. That’s way too warm for insulin or vaccines.
Even the “crisper” drawer isn’t reliable. Freezer coils can cause cold spots that freeze meds. One patient in Dallas lost three vials of insulin after they froze solid in the back of the fridge. Thawing didn’t fix them. They were trash.
So where’s the best spot? The middle shelf. Far from the door. Not touching the back wall. Avoid the vegetable bin. Keep it away from the ice maker. If your fridge has a dedicated drink rack, that’s usually the most stable spot.

How to Know If Your Medicine Is Still Good
Visual changes are your first warning sign. If your insulin looks cloudy, clumpy, or has particles floating in it-don’t use it. Even if it was refrigerated, something went wrong. Same with biologics: if the liquid is discolored, bubbly, or has sediment, throw it out.
But here’s the hard truth: you can’t always tell. A medication can lose 30% of its strength and still look perfect. That’s why temperature monitoring matters. A simple digital thermometer with a memory function-like those used for wine or baby bottles-costs less than $30. Place it next to your meds. Check it every morning. If it’s been above 46°F for more than a few hours, assume the drug is compromised.
One patient with rheumatoid arthritis tracked her Humira fridge temps for three months. She discovered her fridge hit 52°F twice a week during the summer. She switched to a dedicated unit. Her flare-ups dropped by 60%.
Dedicated Medication Fridges: Worth the Investment?
Yes-if you’re on insulin, biologics, or multiple refrigerated drugs. A basic medical fridge (like the Whynter FM-50G) costs $150-$300. It’s small, quiet, and holds 5-10 vials. It maintains a steady 3°C-5°C with alarms if temps go out of range. No more guessing. No more frozen vials.
Some people think, “I’ll just use a cooler with ice packs.” That’s risky. Ice packs can freeze meds. And if the cooler warms up during a power outage, you’re in trouble. A better option? A pharmaceutical-grade portable cooler like TempAid MediCool. These use phase-change materials that stay between 36°F and 46°F for up to 48 hours. Perfect for travel.
And if you’re on Medicare or have high-deductible insurance, ask your pharmacy. Some programs offer free or discounted medication fridges. NeedyMeds has distributed over 8,500 thermometers since 2020. Don’t assume you’re on your own.
What to Do During Power Outages
Power goes out? Don’t panic. But act fast.
- Keep the fridge closed. A full fridge stays cold for up to 4 hours. A half-full one? Only 2.
- Move meds to an insulated cooler with ice packs or frozen gel packs. Don’t use loose ice-it can leak and freeze your vials.
- If you have a generator, plug in the fridge immediately. Don’t wait.
- If the power was out for more than 4 hours and you didn’t have a backup, assume your meds are compromised. Call your pharmacist. Don’t risk it.
One diabetic man in Texas lost his insulin during a 12-hour outage. He used a cooler with frozen water bottles. His temps stayed below 50°F. He called his endocrinologist the next day. They told him to use the vials-because the cooler worked. He’s still alive because he had a plan.

Traveling With Refrigerated Medications
Going on vacation? Flying? Road trip? Pack smart.
- Always carry meds in your carry-on. Never check them. Baggage holds can hit 120°F or freeze at 30,000 feet.
- Use a validated travel cooler (TempAid, MedCool, or similar). Test it before you leave.
- Bring extra vials. In case one gets damaged.
- Carry a doctor’s note. TSA allows refrigerated meds, but they may ask questions.
- At hotels, ask for a mini-fridge. Don’t assume the one in the room is clean or calibrated. Bring your own thermometer.
One mom flying with her son’s biologic shot had her cooler broken by baggage handlers. She called the airline, got a replacement cooler delivered to the airport, and saved her treatment. Planning saved her son’s health.
What Happens If You Get It Wrong?
Using a degraded medication isn’t just ineffective-it can be dangerous.
- Insulin that’s lost potency? Blood sugar spikes. Diabetic ketoacidosis. Hospital visits.
- A vaccine that’s too warm? No immunity. You’re unprotected.
- A biologic that’s degraded? Your autoimmune disease flares. You’re back to pain, swelling, fatigue.
The FDA has issued warning letters about this. In 2021, a patient was hospitalized after using insulin that had been left in a hot car. The insulin was still clear. It looked fine. But it didn’t work. That’s the silent danger.
Bottom Line: Don’t Guess. Measure.
Proper storage isn’t about being perfect. It’s about being consistent. You don’t need a $2,500 medical fridge unless you’re on multiple biologics. But you do need to know where your meds are, what the temp is, and what to do when things go wrong.
Start today:
- Check every refrigerated medication label.
- Buy a $25 digital thermometer and place it next to your meds.
- Move them to the middle shelf of your fridge.
- Keep a backup cooler and ice packs ready for power outages.
- Ask your pharmacist: “Is there a written storage guide for this drug?”
Medications that need refrigeration are lifelines. Treat them like one.


Deborah Williams
November 26, 2025 AT 13:41Kaushik Das
November 28, 2025 AT 13:35Aaron Whong
November 30, 2025 AT 04:43Sanjay Menon
December 1, 2025 AT 06:57Cynthia Springer
December 2, 2025 AT 03:33Brittany Medley
December 3, 2025 AT 08:01Marissa Coratti
December 4, 2025 AT 20:09Rachel Whip
December 6, 2025 AT 11:06JAY OKE
December 7, 2025 AT 05:00Amanda Wong
December 7, 2025 AT 21:51Asia Roveda
December 9, 2025 AT 00:19