What Are Topical Steroids?
Topical corticosteroids are medications applied directly to the skin to reduce redness, itching, and swelling caused by conditions like eczema, psoriasis, and contact dermatitis. They’ve been used for over 70 years and remain the most common prescription for skin inflammation in the U.S. Unlike oral steroids that affect your whole body, topical versions work mostly where you put them. Your skin breaks down most of the medicine before it can enter your bloodstream, which makes them much safer for long-term use-when used correctly.
Why Skin Thinning Happens
One of the biggest worries with topical steroids is skin thinning, also called atrophy. This isn’t just a myth-it’s a real risk. When you use a strong steroid for too long, especially on thin skin like the face, inner arms, or groin, it can break down collagen and elastin. That’s what keeps skin firm and flexible. Without it, skin becomes fragile, shiny, and prone to bruising or stretch marks.
It’s not about using steroids once or twice. It’s about how long and how strong. Super-potent steroids (Class I) like clobetasol can cause atrophy in as little as two weeks if used daily on sensitive areas. Even moderate ones like betamethasone can do damage if applied for months without a break. The National Institutes of Health warns that long-term use without medical oversight is the main cause of these side effects.
Potency Matters: Not All Steroids Are the Same
Topical steroids come in seven strength levels, from super-potent (Class I) to low-potency (Class VII). The right one depends on where you’re applying it and how bad your rash is.
- Super-potent (Class I): Clobetasol, betamethasone dipropionate. Used only for severe flares on thick skin like palms or soles. Never on the face.
- High-potency (Class II-III): Triamcinolone, mometasone. Good for moderate eczema on arms or legs. Limit use to 2 weeks max.
- Moderate to low-potency (Class IV-VII): Hydrocortisone 1% (available over-the-counter). Safe for face, eyelids, and children’s skin. Can be used longer under a doctor’s guidance.
Vehicle matters too. Ointments are strongest because they seal in moisture. Creams are next. Gels and lotions are lighter and better for hairy areas. Foams are great for the scalp. Using the wrong form can change how strong the steroid feels-even if the label says the same strength.
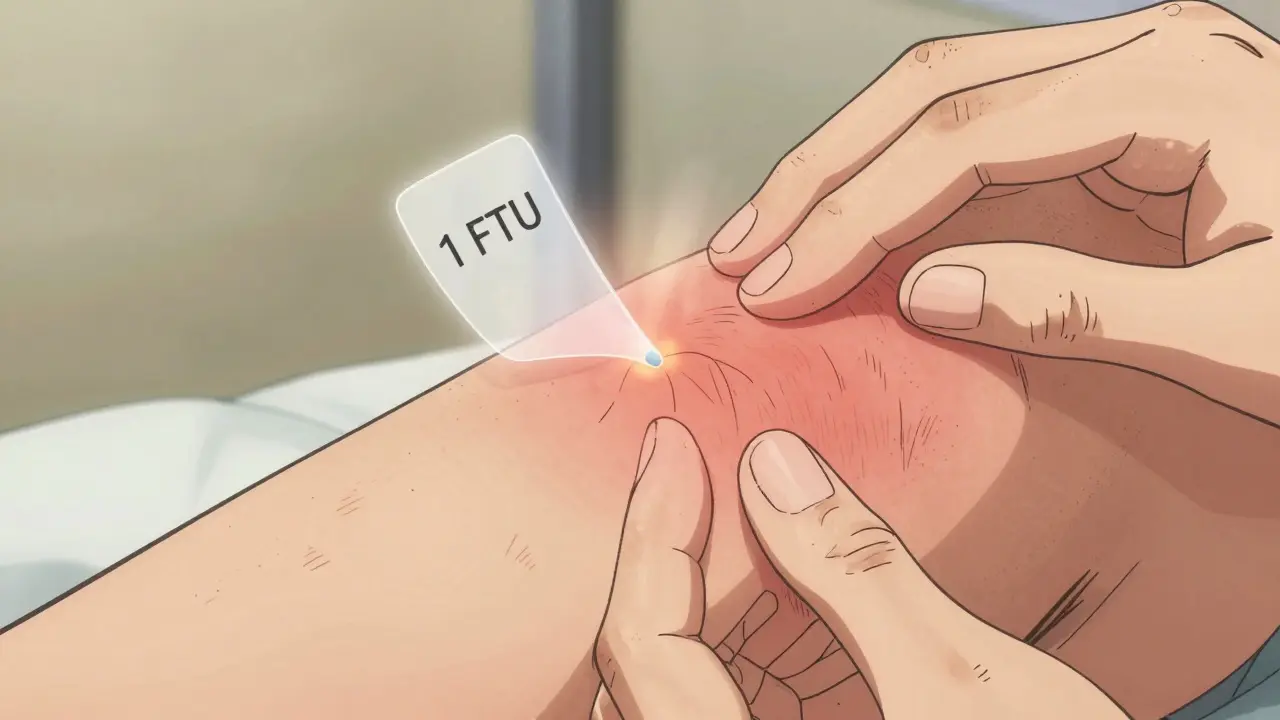
How Much Should You Use? The Fingertip Unit Rule
Most people use too little-or too much. The standard way to measure is the fingertip unit (FTU). One FTU is the amount of cream or ointment that squeezes out from a standard tube along the length of your index finger, from the tip to the first crease.
Here’s what one FTU covers:
- One hand (front and back): 1 FTU
- One arm (front and back): 3 FTUs
- One leg (front and back): 6 FTUs
- One foot: 2 FTUs
- Face and neck: 2.5 FTUs total
That’s it. One FTU is enough for an area the size of two adult palms. Using more doesn’t make it work faster-it just increases your risk of side effects. Studies show patients who use the right amount see results in 7-10 days. Those who underapply often keep using it longer, which increases side effect chances.
Where Not to Use Strong Steroids
Some skin areas are more vulnerable. The face, eyelids, armpits, groin, and breasts have thinner skin and more blood flow. That means more absorption-and more risk.
Guidelines from the UK’s NHS and the American Academy of Family Physicians agree: only mild steroids (like hydrocortisone 1%) should ever go on the face or eyelids. Stronger ones can cause:
- Perioral dermatitis (red bumps around the mouth)
- Acne-like breakouts
- Increased eye pressure leading to glaucoma
- Cataracts with long-term eyelid use
Even if your eczema flares on your cheeks, don’t grab your strongest tube. Use a low-potency steroid for a few days, then switch to a moisturizer. If it doesn’t improve, see a dermatologist.
How Long Is Too Long?
There’s no one-size-fits-all answer, but here’s what experts recommend:
- Super-potent steroids: No more than 2 weeks, and only on thick skin.
- High-potency steroids: Max 2-4 weeks total. Don’t use daily beyond that.
- Moderate to low-potency: Can be used up to 6-8 weeks, but only under supervision.
Doctors often use a “step-down” method: start with a strong steroid to calm the flare, then switch to a weaker one or non-steroidal cream after 1-2 weeks. This gives you quick relief without long-term damage. A 2022 study in the Journal of the American Academy of Dermatology found that 85% of dermatologists use this approach for chronic eczema.
What About Non-Steroid Alternatives?
If you’re worried about skin thinning, there are other options:
- Crisaborole (Eucrisa): A non-steroidal ointment for mild-to-moderate eczema. Safe for face and kids over 2.
- Tacrolimus (Protopic) and Pimecrolimus (Elidel): Creams that calm inflammation without affecting skin structure. Used for sensitive areas.
- Moisturizers with ceramides: Essential for repairing the skin barrier. Use daily, even when you’re not flaring.
These alternatives don’t cause skin thinning, but they’re slower to work and often more expensive. Insurance doesn’t always cover them. That’s why steroids are still first-line-they’re fast, cheap, and effective when used right.
How to Use Them Safely
Follow these steps to avoid side effects:
- Wash your hands before and after applying.
- Apply a thin layer only to inflamed skin-not healthy skin.
- Wait 20-30 minutes before applying moisturizer. If you put moisturizer on first, it dilutes the steroid.
- Use the right potency for the body area.
- Stop after 2-4 weeks unless your doctor says otherwise.
- Don’t cover with bandages unless instructed.
Many people think “more is better.” It’s not. One thin layer works. Rub it in gently until it disappears. If it’s still visible, you used too much.
What If You Already Have Skin Thinning?
If you notice thin, shiny, or bruised skin after long-term steroid use, stop using the product and see a dermatologist. Skin can recover-but it takes time. Recovery can take months to over a year, depending on how long and how strong the steroid was.
Doctors may recommend:
- Stopping the steroid completely
- Switching to a non-steroidal anti-inflammatory
- Using emollients with ceramides to rebuild the skin barrier
- Protecting the area from sun and trauma
Some patients experience withdrawal symptoms-redness, burning, itching-after stopping strong steroids. This is called topical steroid withdrawal. It’s rare but real. It’s not an allergy. It’s your skin adjusting. A dermatologist can help you manage it safely.
Bottom Line: Steroids Are Tools, Not Crutches
Topical steroids aren’t dangerous by nature. They’re powerful tools that help millions of people control painful, itchy skin conditions. The problem isn’t the medicine-it’s how it’s used.
Used correctly, they’re safe. Used carelessly, they can damage skin. The key is matching the strength to the area, using the right amount, and limiting the time. Don’t self-treat for months. Don’t use your leftover steroid cream from last year’s flare. And don’t be afraid to ask your doctor: “Is this the right strength for my skin?”
The future of skin care isn’t avoiding steroids-it’s using them smarter. And that starts with knowing how much to use, where to use it, and when to stop.




Carolyn Whitehead
January 31, 2026 AT 03:24Jodi Olson
February 1, 2026 AT 18:22Gaurav Meena
February 3, 2026 AT 02:18Amy Insalaco
February 4, 2026 AT 08:06Marc Bains
February 5, 2026 AT 17:15Jason Xin
February 5, 2026 AT 22:31Beth Beltway
February 6, 2026 AT 10:24Sheila Garfield
February 8, 2026 AT 04:33Yanaton Whittaker
February 9, 2026 AT 05:10Carolyn Whitehead
February 11, 2026 AT 00:58Sarah Blevins
February 11, 2026 AT 02:07Kathleen Riley
February 11, 2026 AT 20:17Shawn Peck
February 13, 2026 AT 17:40