Hypoglycemia Risk Assessment Tool
How likely are you to experience a low blood sugar event?
Answer a few questions to calculate your personalized risk of hypoglycemia. This tool is based on the information in our article about managing hypoglycemia from diabetes medications.
Your Hypoglycemia Risk Assessment
Recommended Action:
When your blood sugar drops below 70 mg/dL, it’s not just a number-it’s a warning. You might feel shaky, sweaty, or suddenly confused. For people taking insulin, sulfonylureas, or other diabetes drugs that boost insulin, this isn’t rare. About 1 in 4 insulin users experience at least one severe low blood sugar event each year. And many don’t see it coming until it’s too late. The good news? You can stop this cycle. You don’t need to stop your meds. You just need a smarter plan.
Which Diabetes Medications Cause Low Blood Sugar?
Not all diabetes drugs are created equal when it comes to hypoglycemia risk. Some are safer than others. If you’re taking one of these, you’re at higher risk:- Sulfonylureas - Glimepiride, glipizide, glyburide. These force your pancreas to make more insulin, no matter what your blood sugar is. About 15-30% of users get low blood sugar each year.
- Meglitinides - Repaglinide, nateglinide. They work fast but fade fast. You have to eat right after taking them. Miss a meal? You’re asking for trouble.
- All types of insulin - From long-acting basal insulin to rapid-acting mealtime insulin. Risk ranges from 20% to 40% yearly, depending on how complex your dosing is.
On the other side, some drugs rarely cause lows:
- Metformin - Less than 5% risk when used alone.
- GLP-1 agonists - Like semaglutide or liraglutide. Under 2% risk.
- SGLT2 inhibitors - Empagliflozin, dapagliflozin. Around 3% risk.
If you’re on insulin or a sulfonylurea, your risk isn’t just about the drug. It’s about how you use it. And that’s where most people go wrong.
Who’s Most at Risk for Severe Hypoglycemia?
It’s not just about the medicine. Your body, age, and lifestyle matter just as much.- Age 65+ - Your body doesn’t bounce back from low blood sugar like it used to. Risk jumps 40% after 65.
- Long-term diabetes - After 15 years, 10% of type 2 and 25% of type 1 patients develop hypoglycemia unawareness. That means no warning signs. You just pass out.
- Kidney problems - If your eGFR is below 60, your body can’t clear insulin or sulfonylureas properly. Risk doubles.
- Beta-blockers - If you take these for high blood pressure or heart issues, they block the shakes, sweat, and racing heart that warn you of low blood sugar. You’re flying blind.
- Alcohol - Even one drink can shut down your liver’s ability to release glucose. In people under 40, alcohol causes 22% of severe lows.
These aren’t hypotheticals. A 72-year-old with kidney disease on glimepiride who drinks beer on weekends? That’s a perfect storm. And it’s more common than you think.
The 15-15 Rule: Why It Works (and Why Most People Fail)
The standard advice is simple: eat 15 grams of fast-acting sugar, wait 15 minutes, check again. Repeat if needed. Sounds easy. But here’s what actually happens:- 42% of people use candy bars or cookies - too much fat, too slow. Blood sugar stays low.
- 38% use artificial sweeteners - zero carbs. Zero help.
- 29% don’t recheck. They assume they’re fine after one snack.
Here’s what actually works:
- Take 15 grams of pure glucose - that’s 3-4 glucose tablets, 4 oz of regular soda (not diet), or 1 tablespoon of honey.
- Wait 15 minutes. No more snacking. No checking early.
- Test again. If still below 70, repeat.
- Once above 70, eat a snack with protein and carbs - like peanut butter on toast - to prevent another drop.
Studies show this method works in 89% of cases - if done right. But 63% of people get it wrong. Why? Because they don’t have the right stuff on hand.
What to Carry: Real Gear for Real Life
You wouldn’t drive without a spare tire. Don’t manage diabetes without the right tools.- Glucose tablets - Keep them in your car, purse, desk drawer, and jacket. Each tablet is 4g. Buy 20-count packs ($8-$12). They’re cheap, portable, and exact.
- Glucagon emergency kit - If you pass out or can’t swallow, someone needs to give you a shot. New options like Baqsimi (nasal spray) are easier than old injectable kits. Cost: $250. Medicare covers it now.
- Continuous Glucose Monitor (CGM) - Dexcom G7 or Freestyle Libre 3. These alert you before you hit 70. They cut severe lows by 48%. Monthly cost: $89-$130. Medicare covers CGMs for all insulin users since 2023.
- Smart insulin pen - Pens like InPen track your doses and warn you if you’re about to overdose. Cost: $150 upfront, $50/month for sensors. Helps avoid accidental over-dosing.
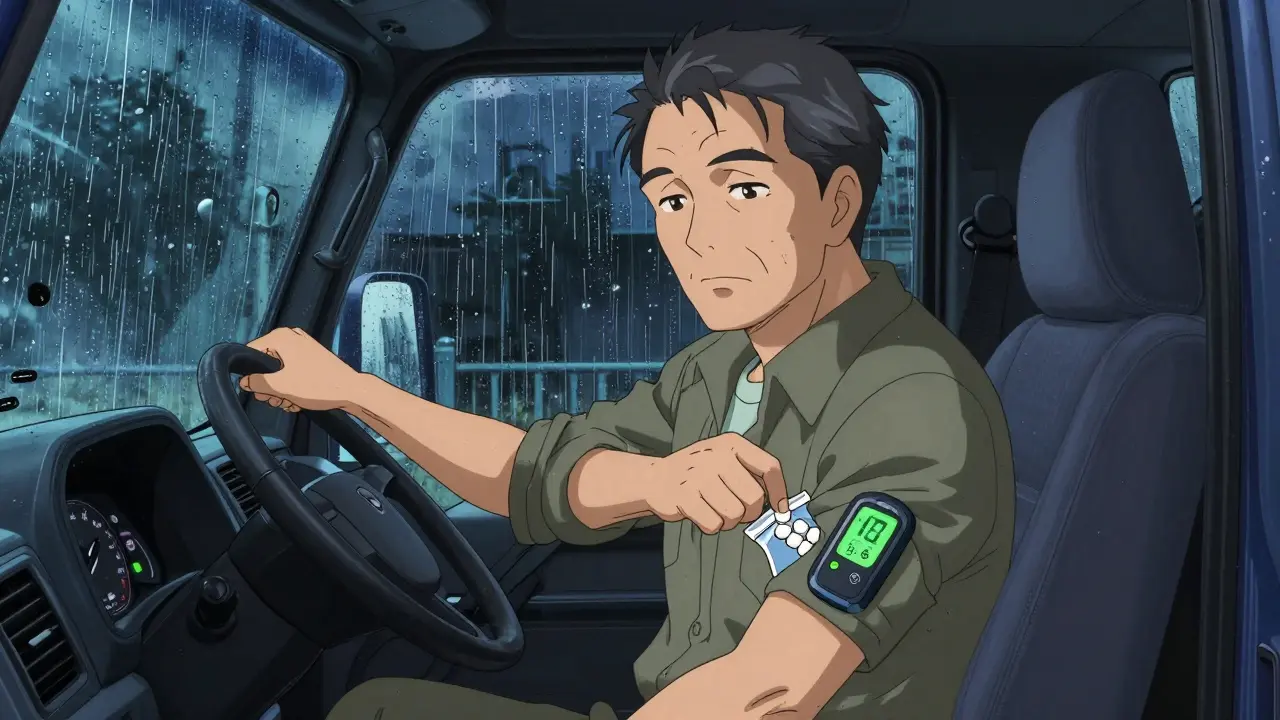
One patient in Dallas, 68, used to have 3-4 lows a week. After getting a CGM and keeping glucose tablets in his truck, his lows dropped to one every 6 weeks. He didn’t change his meds. He just changed his tools.
Why Your Blood Sugar Log Matters More Than You Think
Most people log their blood sugar like a chore. That’s why it fails.Successful users log everything:
- Time of each reading
- Medication taken (name and dose)
- What and when you ate
- Exercise type and duration
- Alcohol consumption
- How you felt (shaky? dizzy? no symptoms?)
The Joslin Diabetes Center found that people who used this detailed log reduced their lows by 52% in three months. Why? Because patterns show up.
Example: A man noticed he always went low at 2 a.m. He was on long-acting insulin. His doctor switched him from Lantus to Tresiba - a longer-acting insulin with less peak. His nighttime lows vanished.
Or: A woman had lows after walking her dog. She started eating 10g of carbs before walks. Done.
If you’re not logging, you’re guessing. And guessing kills.
When to Talk to Your Doctor - And What to Ask
Don’t wait for a crisis. Bring this up at every visit:- “Am I on the safest drug for my risk level?” - If you’re over 65, have kidney issues, or get frequent lows, ask if you can switch from a sulfonylurea to a GLP-1 agonist or SGLT2 inhibitor.
- “Can I try a CGM?” - Even if you don’t think you need it. It’s not just for insulin users anymore. Medicare covers it for anyone on insulin.
- “Do I need a glucagon kit?” - If you live alone, drive, or have kids, yes. Ask for training.
- “Can we adjust my target?” - The ADA now says older adults and those with hypoglycemia unawareness should aim for 80-130 mg/dL - not 70. Your HbA1c might be higher, but you’ll live longer.
One patient told her doctor she was skipping meals because she was scared of lows. Her doctor switched her from glipizide to metformin. Her lows stopped. Her energy improved. She didn’t lose control of her diabetes.
What Not to Do
Avoid these common mistakes:- Skipping meals - It’s tempting, but your body still needs fuel. Use smaller portions. Eat carbs with protein.
- Ignoring nighttime lows - They’re silent. Set an alarm to check at 2 a.m. if you’re at risk.
- Using “sugar-free” products - They don’t help. Only glucose, sucrose, or fructose work.
- Drinking alcohol without food - Always pair it with a snack. Never on an empty stomach.
- Turning off CGM alarms - 62% of pump users do this. Don’t. You’re trading safety for comfort.
What’s Changing in 2026
The tools are getting smarter:- Dasiglucagon (Zegalogue) - New liquid glucagon. No mixing. Just spray or inject. Ready in 10 seconds.
- AI insulin dosing - Trials in 2024 are showing 60% fewer lows with smart algorithms. Expect these to hit clinics by 2026.
- Medicare coverage - Now includes CGMs for all insulin users. No more fighting insurers.
- Smart pens - More affordable. Some now sync with apps and warn you if you’ve taken too much.
These aren’t sci-fi. They’re here. And they’re changing lives.
Final Thought: Safety Isn’t About Perfection
You don’t need perfect blood sugar. You need stable blood sugar. You don’t need to hit HbA1c <7%. You need to avoid passing out, falling, or going to the ER.Start with one change: Keep glucose tablets in your wallet. Set a phone alarm for your next meal. Talk to your doctor about your risk. You don’t have to live in fear. You just have to be prepared.