Drug Label Knowledge Quiz
Test Your Drug Label Knowledge
This quiz helps you identify and understand the key sections of FDA drug labels. Each question focuses on important information from the article.
When you or a loved one is prescribed a new medication, the label that comes with it isn’t just a piece of paper-it’s a legal document packed with life-saving details. But most people never read past the name and dosage. That’s dangerous. The U.S. Food and Drug Administration (FDA) spends years reviewing every drug before it hits the market, and the label is the final, official record of what it can and can’t do. If you don’t know how to read it, you’re flying blind.
The FDA Drug Label Isn’t What You Think
The FDA drug label, officially called the United States Prescribing Information (USPI), isn’t a simple bottle sticker. It’s a highly structured, legally binding document that every prescriber and pharmacist must follow. It’s divided into three main parts: the Highlights, the Table of Contents, and the Full Prescribing Information (FPI). The Highlights section is just half a page-designed to give you the most urgent info fast. But here’s the catch: it’s incomplete. The FDA requires it to say so right on the page. If you stop there, you’re missing up to 95% of the critical details.
The Full Prescribing Information is where the real work happens. It’s broken into 17 numbered sections, each with strict content rules. This format was mandated in 2006 and updated as recently as March 2024. The goal? To make life-or-death information easier to find, not bury it in dense paragraphs. But even with this structure, most people don’t know where to look.
Section 1: Indications and Usage
This is where you find out exactly what the drug is approved for. Not what your doctor thinks it might help with. Not what you read online. Only what the FDA has reviewed and approved. For example, a drug might be approved for treating high blood pressure in adults-but not for children, or for heart failure. If your doctor prescribes it for something off-label, that’s legal, but it’s not listed here. Always check this section first to confirm the drug matches your diagnosis.
Section 2: Dosage and Administration
This is the most commonly misread section. It doesn’t just say “take one pill daily.” It tells you how to adjust the dose for kidney problems, liver disease, elderly patients, or kids. It also specifies if the drug must be taken with food, on an empty stomach, or at a specific time of day. A 2022 Mayo Clinic study found that 38% of dosing errors came from ignoring these details. For example, some antibiotics must be taken two hours before or after dairy products. Miss that, and the drug won’t work. The March 2024 update specifically tightened wording around dose adjustments for renal and hepatic impairment-so if you’re reading an older label, check for updates.
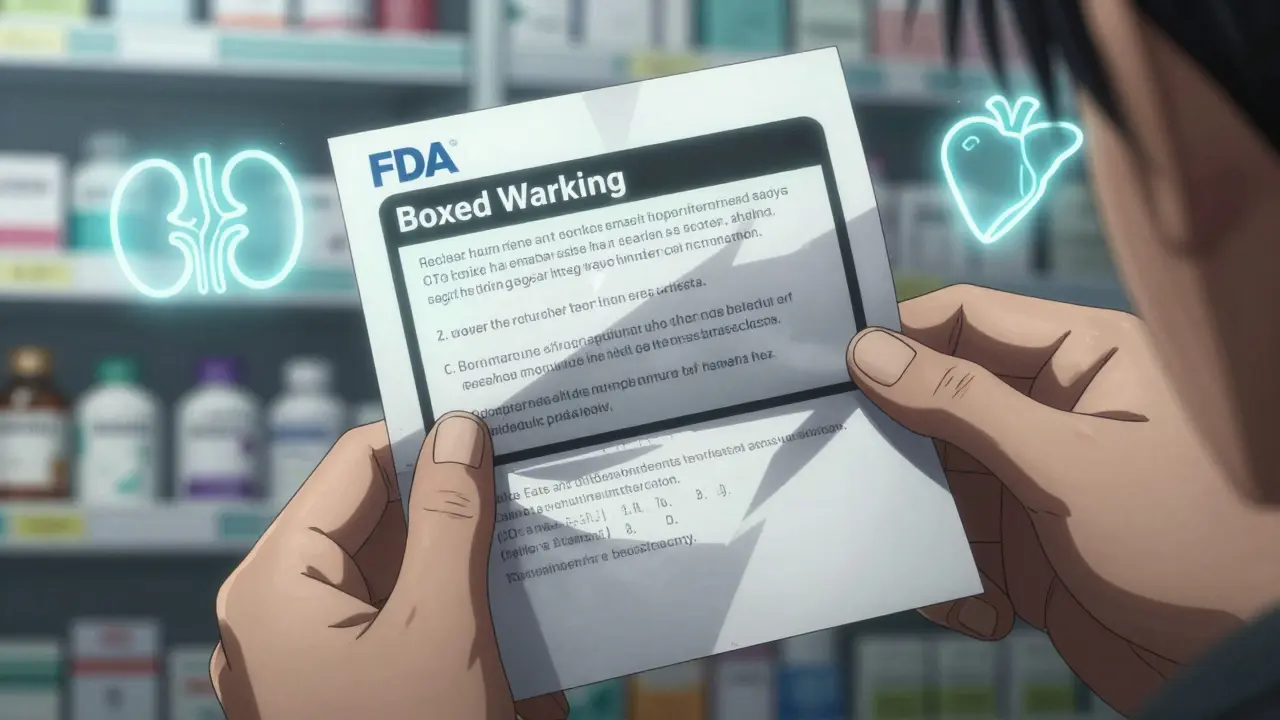
Section 5: Warnings and Precautions (Including the Boxed Warning)
This is the most important section for safety. Look for the Boxed Warning-a thick black border at the top of this section. It’s the FDA’s strongest alert. It means the drug can cause serious harm or death if used incorrectly. Common Boxed Warnings include risks of liver failure, suicidal thoughts, or life-threatening infections. If you see one, don’t skip it. Read every line. These aren’t hypothetical risks-they’re based on real patient data. The FDA requires this warning to be the first thing you see, because it’s often the difference between safe use and tragedy.
Section 6: Adverse Reactions
This section lists side effects, but not like a scary grocery list. It tells you how often they happen. “Common” means more than 1 in 10 people. “Uncommon” is 1 in 100 to 1 in 1,000. “Rare” is less than 1 in 1,000. If a side effect is listed as “rare,” it doesn’t mean it won’t happen to you-but it’s unlikely. Don’t panic over every listed reaction. But if you see something you’re experiencing and it’s marked as “common” or “frequent,” talk to your doctor. Don’t assume it’s just “normal.”
Section 7: Drug Interactions
This section tells you what other drugs, supplements, or even foods can make the medication dangerous. For example, statins (cholesterol drugs) can cause muscle damage when taken with grapefruit juice. Or blood thinners like warfarin can become deadly if you start taking St. John’s Wort. The FDA requires this section to list interactions by severity. Pay attention to the words “contraindicated” (never mix) and “monitor closely” (watch for symptoms). Many patients don’t tell their doctors about vitamins or herbal supplements-this section is why that’s risky.
Section 8: Use in Specific Populations
Is the drug safe if you’re pregnant? Breastfeeding? Over 65? Under 18? This section answers those questions. It’s not just “avoid in pregnancy.” It tells you what the data shows: “No human data available,” “risk cannot be ruled out,” or “no increased risk observed.” For older adults, it may say “dose reduction recommended due to decreased kidney function.” If you’re in one of these groups, this section is non-negotiable. The FDA requires this info because older patients, pregnant women, and children often react differently-and they’re more vulnerable to side effects.
Section 16: How Supplied/Storage and Handling
This looks boring, but it’s vital. It lists the exact form of the drug-tablet, capsule, liquid-and the strength. It also gives you the National Drug Code (NDC), a 10-digit number broken into three parts: labeler code, product code, and package code. This number is how pharmacies and insurers identify your exact medication. If you switch pharmacies and get a different-looking pill, check the NDC. If it doesn’t match, you might have a look-alike/sound-alike error. According to the Institute for Safe Medication Practices (ISMP), these errors cause 12.7% of dispensing mistakes. Also, this section tells you how to store the drug-some need refrigeration, others must be kept away from light. Improper storage can make the drug ineffective or even toxic.
Section 17: Patient Counseling Information
This is the only section written for patients, not doctors. It’s meant to be read aloud by your pharmacist or nurse. It tells you exactly what to say to your patient: “Take this with food to avoid nausea,” “Do not drive until you know how it affects you,” “Use birth control while taking this.” Yet, a 2024 national audit found only 38.2% of providers use this section in real conversations. That’s a missed opportunity. This section is written in plain language for a reason. Use it to ask questions: “What should I watch for?” “What if I miss a dose?” “Is there a cheaper version?”
How to Use This in Real Life
Here’s how to read the label in under five minutes:
- Check the Boxed Warning first. If there’s one, pause. Understand the risk.
- Go to Section 1. Is this drug approved for your condition?
- Jump to Section 2. Are you taking the right dose? Any adjustments for your health?
- Look at Section 7. Are you on any other meds, supplements, or drinking grapefruit juice?
- Check Section 8. Are you pregnant, over 65, or a child?
- Verify the NDC code in Section 16. Does it match your last prescription?
- Read Section 17 out loud. What does it say you should do?
Don’t wait for your doctor to explain it. Don’t assume the pharmacist will tell you everything. The label is your best defense. The FDA designed it so you can find critical info in seconds-if you know where to look.
What’s Changing Now
The FDA is pushing for more patient-friendly labels. In January 2024, they launched the “Labeling for Better Care” initiative. By 2025, new drugs may include interactive digital labels you can scan with your phone. These could show videos, animations, or tailored alerts based on your age or conditions. But until then, the paper label is still the law. And it’s still the most reliable source.
Also, every label now includes a “Recent Major Changes” section. If your drug was updated in the last six months, it’ll list which sections changed. That’s new since 2018-and it’s powerful. A 2024 study showed this feature cut the time between safety updates and clinical use by 35%. Always check this before refilling a prescription.
What Happens If You Ignore It
In 2023, the FDA issued 47 warning letters to drugmakers for labeling errors. That’s not just paperwork-it’s a sign of real danger. When labels are wrong or unclear, patients get the wrong dose, take dangerous combinations, or miss critical warnings. The result? Emergency rooms, hospitalizations, even deaths. A 2020 NCBI analysis found over half of medication errors tied to labeling problems. You don’t need to be a doctor to prevent one. You just need to know how to read the label.
Can I trust the Highlights section alone?
No. The Highlights section is designed to give you a quick snapshot, but it’s intentionally incomplete. The FDA requires it to state that it doesn’t contain all the information. Skipping the Full Prescribing Information means you’re missing critical details about dosing, interactions, and risks. Always read the full label.
What should I do if I don’t understand part of the label?
Ask your pharmacist or doctor. Don’t guess. Pharmacists are trained to interpret FDA labels and can explain Section 2 (Dosage) or Section 7 (Interactions) in plain language. If you’re unsure about a Boxed Warning or NDC code, get it clarified before taking the drug. Your safety depends on it.
Why do the same drugs look different in different pharmacies?
That’s because different manufacturers make generic versions. The active ingredient is the same, but the shape, color, or markings change. Always check the NDC code in Section 16. If the NDC matches your prescription, it’s the correct drug. If it doesn’t, ask your pharmacist why it changed.
How often are FDA drug labels updated?
On average, every 14.3 months. The FDA requires manufacturers to update labels within 30 days of new safety data. Always check the “Recent Major Changes” section before refilling. If you haven’t seen a new label in over a year, it might be outdated.
Is the FDA drug label the same as the patient package insert?
No. The patient package insert is a simplified version meant for consumers. The FDA drug label (USPI) is the full, legally binding document used by healthcare professionals. The patient insert may leave out dosing adjustments, drug interactions, or Boxed Warnings. Always ask your provider for the full label if you want complete information.
Next Steps for Patients and Caregivers
Start today. Print out the Full Prescribing Information for any new prescription you get. Keep it in a folder with your other medical records. When your doctor changes your medication, don’t just take the pill. Ask for the label. Read Section 1, 2, 5, and 17. Write down your questions. Bring them to your next appointment.
If you’re caring for an elderly parent or someone with multiple medications, sit down with them and go through each label together. Use the NDC codes to track what they’re taking. Check the “Recent Major Changes” section every few months. This simple habit can prevent hospital visits, dangerous interactions, and even save a life.
The FDA didn’t create this system to confuse you. It was built to protect you. But protection only works if you use it.




Crystel Ann
January 16, 2026 AT 00:48Finally, someone broke this down without jargon. I printed the full label for my mom’s blood pressure med last week and found a boxed warning I’d never heard of. We called her pharmacist right away-turns out her other supplement was a no-go. This saved her from a hospital trip.
ellen adamina
January 17, 2026 AT 08:44Section 17 is the real MVP. My pharmacist read it to me when I got my new antidepressant and I cried because no one ever explained it that clearly before. Why don’t more doctors do this?
Jan Hess
January 18, 2026 AT 19:59Just read the highlights and moved on for years until my dad had a bad reaction. Turns out his kidney numbers were low and the dose wasn’t adjusted. Now I check every label like it’s a bomb defusal manual. Seriously, this is life or death stuff
Haley Graves
January 19, 2026 AT 01:56Stop letting your doctor be your only source of truth. The label is your legal right to know. Print it. Highlight it. Bring it to every appointment. If they roll their eyes, find a new provider. Your body isn’t a suggestion box.
Nicholas Urmaza
January 20, 2026 AT 20:16People think the FDA is some bureaucratic monster but this system? It’s one of the few things actually working. The Boxed Warning isn’t a scare tactic-it’s a shield. If you ignore it you’re not being bold you’re being reckless
Frank Geurts
January 22, 2026 AT 09:06It is imperative to underscore that the United States Prescribing Information, as codified by the Food and Drug Administration, constitutes the sole authoritative source of pharmacological guidance, and any deviation from its directives constitutes a breach of professional and ethical standards. The patient package insert, while convenient, is inherently insufficient for informed decision-making, as it omits critical pharmacokinetic and contraindication data mandated by federal regulation. Therefore, it is not merely advisable-it is obligatory-that all stakeholders consult the full labeling documentation prior to administration.
Diane Hendriks
January 23, 2026 AT 18:22Why are we letting corporations dictate how we take medicine? The FDA doesn’t care about you-they care about liability. The ‘Recent Major Changes’ section? That’s not transparency-it’s damage control after another death. The system is rigged. You think reading the label saves you? It just makes you complicit in a broken machine.
RUTH DE OLIVEIRA ALVES
January 25, 2026 AT 05:38As a healthcare professional with over two decades of experience, I have consistently advocated for patient empowerment through direct engagement with the United States Prescribing Information. The structural clarity introduced in the 2006 revision, further refined in March 2024, represents a monumental advancement in pharmacovigilance. I encourage all individuals to treat the Full Prescribing Information not as an obstacle, but as a covenant of safety between regulatory authority and the individual. The NDC code, in particular, serves as an indispensable verification tool against pharmaceutical substitution errors, which remain among the most preventable causes of iatrogenic harm.
Gloria Montero Puertas
January 26, 2026 AT 01:23Oh, wow. Someone finally wrote something that doesn’t sound like it was generated by a ChatGPT bot trying to win a ‘Most Boring Post of the Year’ award. And yet-you’re still missing the point. You think reading the label makes you smart? It just means you’re not completely incompetent. The real tragedy is that this information exists at all-because the pharmaceutical industry should never have been allowed to sell drugs without mandatory, plain-language, animated, voice-guided, interactive, multilingual, culturally-adapted, trauma-informed, AI-driven, real-time safety alerts embedded directly into your smart fridge. And yet here we are. Reading PDFs. In 2024. Pathetic.