What Exactly Is Pharmacist Substitution Authority?
Pharmacist substitution authority isn’t just about swapping a brand-name pill for a cheaper generic. It’s a growing set of legal powers that let pharmacists make real clinical decisions-like changing a medication, starting a new treatment, or even prescribing certain drugs-without waiting for a doctor’s approval. This isn’t theoretical. In 2025, 12 states passed new laws expanding what pharmacists can do, and over 200 bills are still under review across the country. The goal? Fix gaps in care, especially in places where doctors are hard to find.
Generic Substitution: The Baseline Everyone Has
Every state lets pharmacists swap a brand-name drug for a generic version if the doctor didn’t write “dispense as written.” This isn’t new. It’s been standard since the 1980s. But even this simple power has rules. The generic must be FDA-approved as therapeutically equivalent. That means it works the same way, has the same active ingredient, dose, and strength. Pharmacists check this every time. If a patient asks why they got a different pill, the pharmacist should explain it’s not a different medicine-just a lower-cost version of the same thing.
Therapeutic Interchange: When Pharmacists Can Change Drug Classes
Some states go further. In Arkansas, Idaho, and Kentucky, pharmacists can swap one drug for another in the same therapeutic class-even if they’re not chemically identical. For example, switching from one blood pressure medication to another if the first one isn’t working or is too expensive. But it’s not automatic. The doctor must write something like “therapeutic substitution allowed” on the prescription. If they don’t, the pharmacist can’t change it. And even when allowed, the pharmacist must tell the patient what’s changing, why, and get their okay. They also have to notify the original prescriber. This keeps the patient’s medical record accurate and gives the doctor a chance to object if needed.
Prescription Adaptation: Fixing Prescriptions Without a Doctor Visit
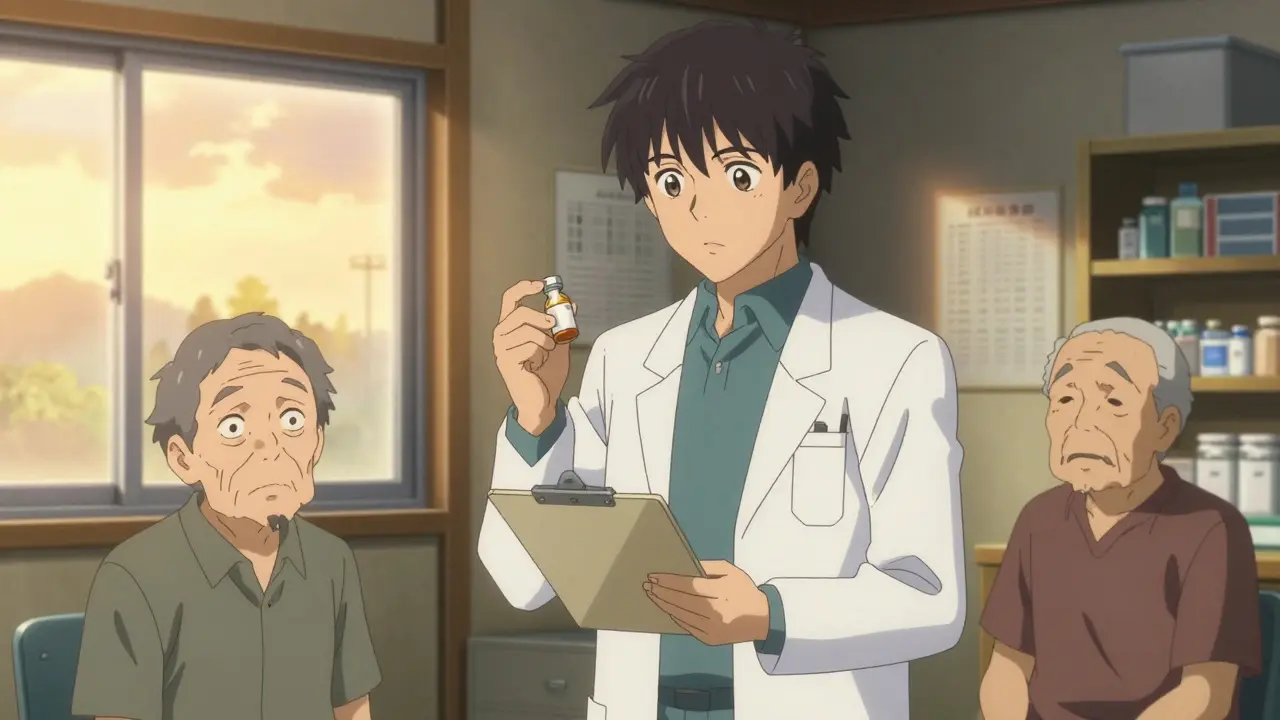
Imagine you live in a rural town with no nearby clinic. Your blood sugar is too high, and your diabetes med needs adjusting. Normally, you’d need to drive hours to see your doctor. In states that allow prescription adaptation, your pharmacist can change the dose, refill it early, or switch to a better option-without calling the doctor first. This is legal in about half the states. The pharmacist must follow strict protocols: check your history, make sure it’s safe, document everything, and inform your doctor afterward. It’s not about replacing doctors. It’s about removing unnecessary barriers for people who can’t easily get care.

Collaborative Practice Agreements: The Hidden Backbone of Expanded Care
Most of the big changes in pharmacist authority come through Collaborative Practice Agreements (CPAs). These are formal, written contracts between pharmacists and physicians or other providers. They spell out exactly what the pharmacist can do: test for flu, adjust warfarin doses, prescribe nicotine patches, or manage asthma. CPAs exist in all 50 states and D.C., but how they work varies wildly. In some places, the doctor controls every decision. In others, the pharmacist runs the show under clear guidelines. The trend? More autonomy for pharmacists. New CPAs are being written with fewer doctor signatures and more pharmacist-led protocols. That’s a big shift-from pharmacist as dispenser to pharmacist as clinical partner.
State-by-State Differences: Who Can Do What?
There’s no national standard. Each state sets its own rules. Maryland lets pharmacists prescribe birth control to adults. Maine lets them hand out nicotine patches without a prescription. California uses the word “furnish” instead of “prescribe” to avoid legal pushback from doctors. New Mexico and Colorado let their boards of pharmacy create statewide protocols-so if a new treatment becomes standard, pharmacists can start offering it without waiting for a new law. Meanwhile, some states still only allow generic swaps. This patchwork makes it confusing for patients and pharmacists alike. But it also means innovation is happening fast in some places, while others lag behind.
Why This Matters: Access, Equity, and Shortages
Over 60 million Americans live in areas with too few doctors. In those places, pharmacists are often the most accessible health professionals. A 2023 report from the Health Resources and Services Administration found that in rural communities, pharmacists are the first point of contact for chronic disease management. When pharmacists can prescribe emergency contraception, flu shots, or adjust insulin doses, patients get care faster. That’s not just convenient-it’s lifesaving. The American College of Clinical Pharmacy says pharmacist-led medication management improves outcomes, reduces hospital visits, and cuts costs. But without reimbursement, many of these services can’t survive. Insurance companies still don’t always pay pharmacists for clinical work, even when the law lets them do it.
The Big Hurdle: Insurance Doesn’t Pay
Just because a state lets a pharmacist prescribe doesn’t mean Medicare or private insurers will pay for it. Most insurance plans still only reimburse for dispensing drugs-not for counseling, testing, or adjusting meds. That’s why the federal ECAPS Act (Ensuring Community Access to Pharmacist Services) is so important. If passed, it would force Medicare Part B to cover pharmacist services like screenings, vaccinations, and chronic disease management. That could change everything. Private insurers would likely follow. Without reimbursement, pharmacists can’t afford to spend time on clinical work. They’re trained for it. But they can’t stay in business doing it for free.
Opposition and Concerns
Not everyone supports this expansion. The American Medical Association still argues pharmacists aren’t trained like physicians. They worry about safety and oversight. Some fear corporate pharmacies are pushing these changes to boost profits. But data doesn’t back up those fears. Studies from the Journal of the American Pharmacists Association show no increase in adverse events when pharmacists manage medications under protocols. In fact, patient satisfaction goes up. The real issue isn’t training-it’s outdated rules. Pharmacists now get clinical doctorates, complete residencies, and pass board certifications. Their education has evolved. The law just hasn’t caught up everywhere.
What’s Next?
The momentum is clear. More states will expand authority. More pharmacists will be able to prescribe. More patients will get care without long waits. The next big step is federal reimbursement. If ECAPS passes, it won’t just help pharmacists-it will reshape how primary care is delivered. Pharmacies could become neighborhood health hubs, offering blood pressure checks, diabetes management, and mental health support-all under one roof. That’s not a fantasy. It’s already happening in Minnesota, Oregon, and Washington. The question isn’t whether this will happen. It’s how fast.




Coy Huffman
February 3, 2026 AT 07:06Joy Johnston
February 4, 2026 AT 21:47Amit Jain
February 5, 2026 AT 17:28Keith Harris
February 5, 2026 AT 21:30Kunal Kaushik
February 6, 2026 AT 02:16Roshan Gudhe
February 7, 2026 AT 01:17Prajwal Manjunath Shanthappa
February 8, 2026 AT 17:06Antwonette Robinson
February 9, 2026 AT 23:46Ed Mackey
February 11, 2026 AT 22:07Katherine Urbahn
February 13, 2026 AT 20:21Alex LaVey
February 14, 2026 AT 05:01Justin Fauth
February 16, 2026 AT 01:53Meenal Khurana
February 17, 2026 AT 17:49Shelby Price
February 18, 2026 AT 09:45