Most people throw away pills after the expiration date on the bottle. But what if that’s the only medicine you have when someone’s life is on the line? In a real emergency-during a natural disaster, a sudden shortage, or far from a pharmacy-using an expired medication isn’t just common, it’s sometimes the only choice left.
Expiration Dates Aren’t Kill Switches
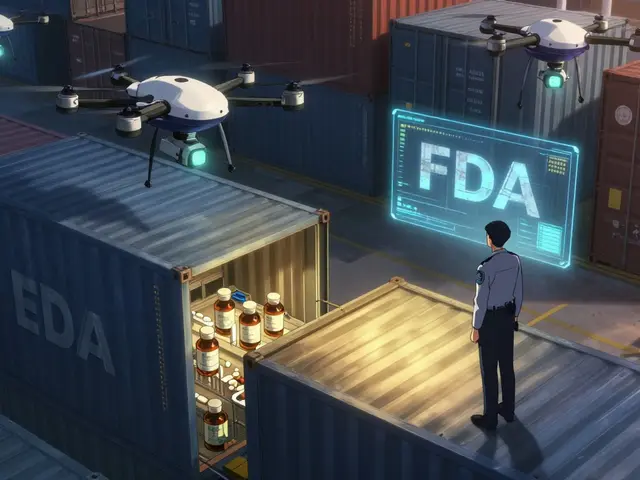
The date printed on your medicine bottle doesn’t mean the drug suddenly turns toxic or useless. It’s a manufacturer’s guarantee: up to that date, the drug will work as intended if stored properly. After that? No one can promise full strength-but that doesn’t mean it’s worthless. The FDA’s Shelf Life Extension Program (SLEP), run since 1985 with the Department of Defense, tested over 100 drugs. Results showed that 90% retained at least 90% of their original potency up to 15 years past expiration. In one study of 122 military stockpiled drugs, 88% were still effective after 8 years. These aren’t outliers. They’re data. Why do companies set such short dates? Legal protection. If a drug fails after two years and someone gets hurt, the manufacturer can point to the expiration date. But the science says: most pills and capsules don’t break down that fast.Not All Medicines Are Created Equal
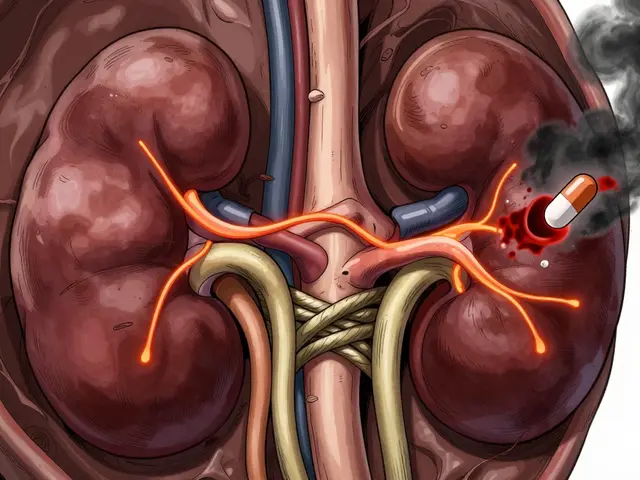
Some expired drugs are low risk. Others could kill you. Low-risk expired meds: Ibuprofen, acetaminophen, diphenhydramine (Benadryl), and aspirin. Studies show these often keep 85-90% potency for 4-5 years past expiration, even in less-than-ideal storage. A 2022 survey found 74% of Americans keep OTC painkillers past their date-and most use them without issue. Moderate-risk expired meds: Seizure medications, blood thinners like warfarin, and thyroid pills. These need precise dosing. A 15% drop in seizure drug potency can increase seizure risk by 35%. A 10% change in warfarin can cause dangerous clots or bleeding. In a true emergency-with no alternatives-these might be used, but only if the patient’s life is at immediate risk. High-risk expired meds: Insulin, epinephrine (EpiPen), nitroglycerin, and liquid antibiotics. These degrade fast. Insulin can lose 20% potency per month at room temperature. Epinephrine loses 25% potency per year. Nitroglycerin breaks down in light and heat. Liquid antibiotics can become ineffective-or worse, toxic. A 2023 FDA safety alert warned that expired insulin glargine lost up to 35% potency after just six months. That’s enough to trigger diabetic ketoacidosis. These aren’t drugs you gamble with.Real-World Emergency Use: Stories from the Field
In 2022, during a nationwide albuterol shortage, Denver Health extended expiration dates by 90 days for over 1,200 inhalers. Zero adverse events were reported. A paramedic in Texas used a 3-month-old expired EpiPen on a patient having an anaphylactic reaction. The patient improved within two minutes. They still went to the ER-standard protocol-but the expired pen worked. But it doesn’t always go right. In 2023, a case report in Prehospital Emergency Care described a child with status asthmaticus who didn’t respond to a 6-month-expired albuterol inhaler. The child ended up intubated. EMS agencies across the U.S. report similar patterns. A 2022 survey by the American Ambulance Association found 43% of providers had used expired meds during shortages. Of those, 89% said outcomes were positive-when used for life-threatening situations with no other options.
When You Should Never Use an Expired Drug
Even in emergencies, some rules are absolute:- Never use expired insulin if you have any alternative-even a different brand or type.
- Never use expired epinephrine if you can get a new one within 10 minutes.
- Never use expired liquid antibiotics. They don’t just weaken-they can grow bacteria or form harmful compounds.
- Never use tetracycline antibiotics after expiration. They can damage kidneys.
How to Safely Assess an Expired Drug in an Emergency
If you’re forced to use an expired drug, follow these steps:- Check the storage history. Was it kept in a cool, dry, dark place? If it was left in a hot car or a steamy bathroom, skip it.
- Inspect visually. Tablets should be intact, not crumbling. Capsules shouldn’t be sticky or leaking. Liquids must be clear-no cloudiness, particles, or color change.
- Know the drug class. Is it a life-saver like epinephrine or a comfort drug like ibuprofen? Use the latter first.
- Use it only when no other option exists. This isn’t a shortcut. It’s a last resort.
- Document everything. Date, time, drug name, lot number, storage conditions, patient response. This matters if things go wrong.



Scottie Baker
January 14, 2026 AT 06:26Look, I’ve used an expired EpiPen in the field. Didn’t kill anyone. The guy lived. The FDA doesn’t live in a van down by the river when the ambulance is 45 minutes away and the kid’s lips are turning blue. You wanna be safe? Fine. But don’t lecture people who are actually doing the work when the system fails.
Gregory Parschauer
January 15, 2026 AT 14:25Oh please. This is the kind of dangerous pseudoscience that gets people killed. You’re glorifying negligence under the guise of "emergency pragmatism." The expiration date exists for a reason - pharmacokinetics, degradation pathways, stability testing. You think your grandma’s aspirin from 2018 is somehow "still 85% potent"? That’s not science, that’s wishful thinking wrapped in a FDA study citation. You’re not a hero. You’re a liability.
Randall Little
January 17, 2026 AT 13:25So let me get this straight - you’re saying if I’m stranded in Alaska with a diabetic relative and the only insulin is 11 months expired, I should just let them die because the FDA says so? Or do I use the vial that might save them, then get sued by a lawyer who’s never held a syringe? This isn’t a debate about chemistry. It’s about moral calculus. The system failed. People are improvising. Stop acting like your inbox is the moral authority.
Robin Williams
January 18, 2026 AT 02:56man i’ve kept benadryl past its date for like 7 years. kept it in the drawer. used it for my kid’s allergy flare. worked like a charm. no weird dreams, no seizures, no magic poison. just sleepy kid. the system is broken. companies wanna make you buy new shit every 2 years. if it looks right, smells right, and you’re not injecting it into your jugular… maybe don’t panic?
laura Drever
January 19, 2026 AT 00:27Priyanka Kumari
January 20, 2026 AT 15:55I work in rural India where pharmacies are 30km away and power cuts last for days. We’ve used expired paracetamol, antihistamines, even antibiotics - carefully, with documentation. No one died. No one got worse. What’s the alternative? Let a child suffer because the date on the bottle says so? Science says potency lasts. Humanity says use it if it helps. We don’t need FDA guidelines to be decent humans.
Damario Brown
January 21, 2026 AT 06:29you guys are missing the point. it’s not about the pill. it’s about trust. if you’re using expired meds, you’re trusting a system that’s been lying to you for decades. the expiration date isn’t science - it’s a legal shield. the real crisis isn’t the meds, it’s that we’re forced to choose between corporate greed and survival. and now we’re being told to feel guilty for choosing survival? that’s the real horror story.
Clay .Haeber
January 21, 2026 AT 07:13Oh wow. A whole 12-page essay on how to not die because Big Pharma doesn’t want you to save money. Next they’ll tell us to use expired toilet paper in a zombie apocalypse. "Just check for stickiness!" Meanwhile, my 2019 Advil is still in the cabinet, next to my 2016 flannel and my hope that capitalism won’t collapse before I need a painkiller. I’ll take my 85% potency over your 100% corporate greed any day.
Anny Kaettano
January 23, 2026 AT 03:22As a nurse who’s worked in three disaster zones, I’ve seen this play out. Expired ibuprofen? Fine. Expired insulin? Don’t. But here’s what no one says: most people don’t know the difference. We need community education - not fear, not jargon, just clear, simple rules. Teach people to check storage, look for discoloration, know which drugs are critical. This isn’t about breaking rules. It’s about giving people the tools to make smart, safe choices when the system fails them.
Lance Nickie
January 23, 2026 AT 13:22Jesse Ibarra
January 24, 2026 AT 10:44You’re romanticizing chaos. This isn’t "survival wisdom." It’s a one-way ticket to a wrongful death lawsuit wrapped in a TikTok bio. You cite FDA data but ignore that 90% potency doesn’t mean 90% safety. A 15% drop in warfarin? That’s not a "slight change." That’s a stroke waiting to happen. And you think the kid who got intubated because of your "emergency" was just unlucky? No. They were the victim of your performative bravery.
John Pope
January 25, 2026 AT 12:39Let’s be real - this whole thing is a performance of moral superiority. You’re not using expired meds because you’re desperate. You’re using them because you want to feel like a rebel. A rugged individualist defying Big Pharma. But here’s the twist: you’re still playing by their rules. You’re still terrified of the expiration date. You’re still scared to admit that the real villain isn’t the pill - it’s the system that made you feel like you had to choose between life and legality. So go ahead. Use your 2018 aspirin. But don’t call it courage. Call it what it is: a symptom of a broken world.