Before 2014, being diagnosed with chronic hepatitis C meant years of painful injections, brutal side effects, and no guarantee you’d be cured. Many people lived with the virus for decades, watching their livers slowly scar, fearing cirrhosis, liver failure, or cancer. Today, that story has changed - completely. If you have chronic hepatitis C, you can now be cured in as little as eight weeks, with almost no side effects, and your liver can begin to heal itself. This isn’t science fiction. It’s what’s happening in clinics across the U.S. right now.
What Chronic Hepatitis C Actually Does to Your Liver
Chronic hepatitis C isn’t just a virus in your blood. It’s a silent attacker on your liver. Over 10, 20, or even 30 years, the virus slowly destroys liver cells, replacing healthy tissue with scar tissue - a process called fibrosis. Left unchecked, fibrosis turns into cirrhosis, where the liver hardens and can’t function properly. At that point, your risk of liver cancer skyrockets. About 1 in 5 people with untreated hepatitis C will develop cirrhosis within 20 years. Many don’t feel sick until it’s too late.
That’s why early detection matters. But here’s the good news: once you’re diagnosed, the game changes. The virus doesn’t have to win. Modern treatments don’t just slow it down - they wipe it out.
The Revolution: Direct-Acting Antivirals (DAAs)
The old treatment for hepatitis C? Pegylated interferon shots and ribavirin pills. You took them for up to 48 weeks. Side effects included severe fatigue, depression, flu-like symptoms, and anemia. Cure rates? Only 40% to 80%, depending on your genotype. Many people couldn’t finish treatment because it was too hard.
Then came DAAs - direct-acting antivirals. These are oral pills that target the virus at its core. They don’t boost your immune system. They don’t make you sick. They attack the virus directly, blocking the proteins it needs to copy itself. There are three main types:
- NS3/4A protease inhibitors - like glecaprevir - stop the virus from making new proteins.
- NS5A inhibitors - like velpatasvir and pibrentasvir - prevent the virus from assembling new copies.
- NS5B polymerase inhibitors - like sofosbuvir - shut down the virus’s RNA replication engine.
These drugs are combined into single pills. You take one or two tablets a day. No shots. No hospital visits. No interferon.
How Effective Are They? The Numbers Don’t Lie
Today’s DAA regimens cure more than 95% of people - even those with cirrhosis, HIV co-infection, or who’ve failed older treatments. For people who’ve never been treated before, cure rates hit 97% to 99%. That’s not an average. That’s nearly every single person.
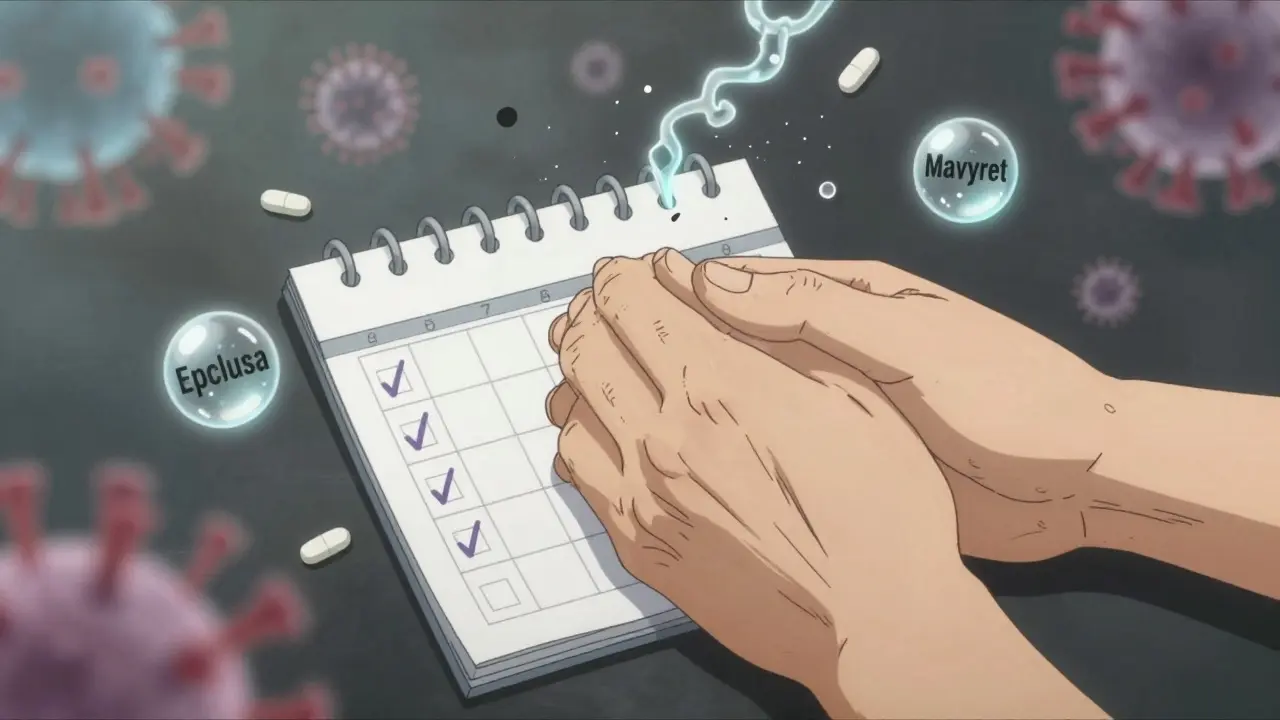
Take Epclusa (sofosbuvir/velpatasvir) or Mavyret (glecaprevir/pibrentasvir). Both are pan-genotypic, meaning they work against all six major strains of hepatitis C. You don’t even need to know your genotype anymore - doctors can start treatment right away. Treatment lasts 8 to 12 weeks for most people. Those with advanced liver disease might need 12 to 24 weeks.
The CDC confirms that these regimens are now the global standard. The World Health Organization recommends them for adults and children as young as 3 years old. In 2023, over 90% of new hepatitis C prescriptions in the U.S. were for DAAs. Interferon is gone - not just outdated, but obsolete.
What Happens to Your Liver After Treatment?
Getting rid of the virus is just the first step. The real win is what happens next: your liver heals.
Studies show that after successful DAA treatment, fibrosis stops progressing in 95% of patients. In 70% of cases, the liver actually regenerates - scar tissue breaks down and is replaced with healthy tissue over time. This isn’t speculation. It’s shown in liver biopsies and non-invasive scans like FibroScan.
One 58-year-old man in Texas, diagnosed with stage 3 fibrosis, completed 12 weeks of Mavyret in 2022. His follow-up scan in 2024 showed stage 1 fibrosis - nearly normal. He didn’t have to change his diet or take supplements. He just stopped the virus. His liver did the rest.
For those who’ve had liver transplants, the results are even more dramatic. Before DAAs, only about 25% of transplant patients cleared the virus. Now, it’s 94%. That means fewer re-transplants, fewer deaths, and more years of life.
Side Effects? Almost None
People expect side effects. They’ve been burned before. But with DAAs, the side effect profile is dramatically different.
Most people feel nothing. A small number report mild fatigue or a headache in the first week. That’s it. No nausea. No hair loss. No depression. No need to quit work or cancel plans.
A Gilead survey of 5,000 patients found 97% would recommend treatment to a friend. 89% said it didn’t affect their daily life. On Reddit’s hepatitis C community, 92% of 1,247 users reported being cured with minimal side effects. One wrote: “Cured in 12 weeks with Epclusa - only side effect was mild fatigue first week.”
Compare that to interferon, where nearly everyone had severe side effects. The difference isn’t just better science - it’s better humanity.
Cost and Access: The Real Hurdle
Yes, the price tag is high. In 2023, a 12-week course of Epclusa or Mavyret cost around $74,700 in the U.S. That’s a lot. But it’s not the $94,500 Sovaldi cost in 2013. Prices have dropped. And here’s what most people don’t know: 70% of uninsured patients get full financial help through manufacturer assistance programs. Medicaid, VA, and many private insurers cover DAAs with little to no out-of-pocket cost.
The real barrier isn’t the drug - it’s getting tested and connected to care. Only 20% of people with hepatitis C globally even know they’re infected. In the U.S., many people - especially those without regular healthcare - never get screened. That’s why the CDC and WHO are pushing for universal testing for adults born between 1945 and 1965, and for anyone with risk factors like past IV drug use or blood transfusions before 1992.
Insurance denials still happen. About 28% of patients face initial denials, but most win their appeals with help from patient advocates. The key is persistence. Don’t take “no” as final.

Who Can Be Treated? Almost Everyone
DAAs work for almost everyone:
- People with cirrhosis
- Those with HIV co-infection
- Patients on dialysis
- People with liver transplants
- Those who’ve failed prior hepatitis C treatment
- Children as young as 3
The only exceptions are rare cases where someone has developed resistance mutations after multiple failed DAA treatments. Even then, newer combinations like Vosevi (sofosbuvir/velpatasvir/voxilaprevir) can still work. Doctors now have backup plans.
What’s Next? Elimination by 2030
The World Health Organization aims to eliminate hepatitis C as a public health threat by 2030. That means reducing new infections by 90% and cutting deaths by 65%. We have the tools. We have the cure. What’s missing is access.
High-income countries like the U.S. and Canada have treated over 60% of diagnosed patients. Low-income countries? Only 15%. Gilead and other manufacturers are now offering generic versions for as little as $50 per course in qualifying countries. That’s the future - cheap, effective, and available to everyone.
In the U.S., the Veterans Health Administration treated 95% of diagnosed veterans. Community clinics? Only 65%. The gap isn’t in medicine. It’s in outreach.
How to Get Started
If you think you might have hepatitis C - or if you’ve ever used IV drugs, had a blood transfusion before 1992, or were born between 1945 and 1965 - get tested. A simple blood test can tell you if you’re infected.
If you test positive, don’t wait. Ask your doctor about DAA treatment. You don’t need a liver specialist. Primary care doctors can manage 85% of cases. Bring up Epclusa or Mavyret by name. If your insurance denies it, ask for help from a patient advocate. Many hospitals have them.
Once you start, take your pills every day. Don’t skip. Complete the full course. Then get your follow-up test at 12 weeks. That’s when they check for SVR - sustained virologic response. If it’s undetectable, you’re cured.
And then? Your liver gets to heal. Your risk of cancer drops. You can hug your kids without fear. You can date, marry, have a family. You can live - not just survive.
Can chronic hepatitis C be cured?
Yes. With modern direct-acting antivirals (DAAs), more than 95% of people with chronic hepatitis C can be cured in 8 to 12 weeks. Cure means the virus is undetectable in the blood 12 weeks after treatment ends - called a sustained virologic response (SVR). Once cured, the virus does not return.
Do hepatitis C treatments damage the liver?
No. In fact, they protect it. DAAs stop the virus from attacking the liver. Once the virus is cleared, the liver begins to repair itself. Studies show fibrosis stops progressing in 95% of patients, and 70% see actual regression of scar tissue within five years. The treatment doesn’t harm the liver - it gives it a chance to heal.
Are there side effects with modern hepatitis C drugs?
Most people have no side effects. A small number report mild fatigue or a headache during the first week. Unlike older interferon treatments, DAAs don’t cause depression, hair loss, anemia, or flu-like symptoms. Over 90% of patients experience no significant side effects, according to CDC data.
Can I get hepatitis C again after being cured?
Yes, but it’s rare. Being cured doesn’t make you immune. If you’re exposed again - for example, through sharing needles or unsterile tattoos - you can get infected again. The good news is, if you do, you can be cured again. The same treatments work a second time.
Do I need to avoid alcohol after being cured?
Yes. Even after you’re cured, your liver may still have some scarring. Alcohol can cause further damage and increase your risk of liver cancer. Doctors recommend avoiding alcohol completely, especially if you had cirrhosis before treatment. The liver has healed, but it still needs protection.
How do I know if my treatment worked?
You’ll get a blood test 12 weeks after finishing your last pill. This test checks for HCV RNA. If the virus is undetectable, you’ve achieved a sustained virologic response (SVR), which means you’re cured. This result is permanent - the virus won’t come back on its own.
Is hepatitis C treatment covered by insurance?
Most insurance plans, including Medicaid and Medicare, cover DAA treatment. Some require prior authorization, and a small number of patients face initial denials. But with help from patient advocacy programs or your doctor’s office, over 90% of denials are overturned. Manufacturer assistance programs also cover 70% of uninsured patients.


Hilary Miller
January 22, 2026 AT 12:30Neil Ellis
January 23, 2026 AT 10:49Malik Ronquillo
January 24, 2026 AT 01:49Akriti Jain
January 24, 2026 AT 16:54Sarvesh CK
January 25, 2026 AT 20:32Margaret Khaemba
January 26, 2026 AT 03:15arun mehta
January 26, 2026 AT 07:17Alec Amiri
January 27, 2026 AT 01:28Brenda King
January 28, 2026 AT 04:38Ryan Riesterer
January 28, 2026 AT 05:40Kenji Gaerlan
January 30, 2026 AT 03:57Chiraghuddin Qureshi
January 30, 2026 AT 18:28Daphne Mallari - Tolentino
February 1, 2026 AT 08:16