Did you know that nearly half of all people taking medication for chronic conditions like high blood pressure, diabetes, or heart disease miss doses-sometimes regularly? It’s not laziness. It’s forgetfulness, confusion, or just too many pills at too many times. And it’s costing the U.S. healthcare system over medication adherence $300 billion a year. But there’s a simple, powerful fix: medication reminder apps.
Why Medication Reminder Apps Actually Work
Traditional methods-pills in a box, sticky notes, alarm clocks-don’t cut it anymore. People forget. Life gets busy. Side effects make you want to skip a dose. But apps? They’re built to fight that. They don’t just buzz at the right time. They track what you took, remind you when you miss, and even tell you why it matters.
A 2025 review of 14 top apps found that 10 out of 14 showed real, measurable improvements in adherence. Patients using these apps were about twice as likely to take their meds as prescribed compared to those who didn’t. That’s not small. That’s life-changing.
What makes them better than a simple alarm? Personalization. Apps like Medisafe and MyTherapy let you set different times for different pills, add photos of your meds, and even log how you’re feeling. Some use AI to predict when you’re likely to skip a dose based on your past behavior. Others give you little rewards or progress bars to keep you motivated.
Top Medication Reminder Apps in 2025
Not all apps are created equal. Here are the five most effective, widely used, and trusted options right now:
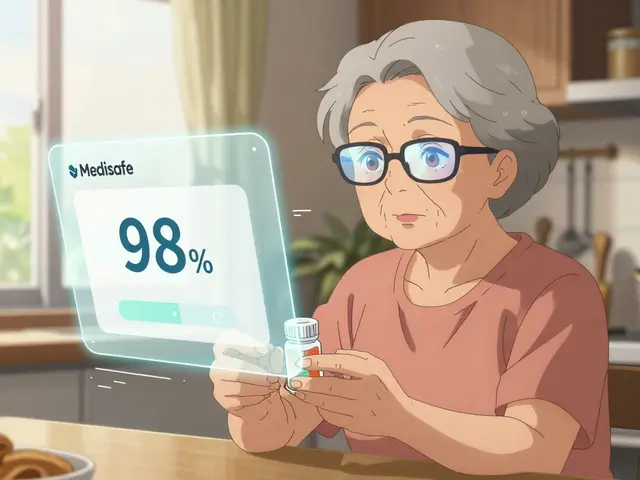
- Medisafe: The most downloaded app in this space. Works on iOS and Android. Lets you add photos of your pills, sync with family members, and get alerts if you miss a dose. Integrates with some pharmacy systems and EHRs via FHIR. 4.7/5 on iOS as of June 2025.
- MyTherapy: Strong on tracking and reporting. You can log symptoms, mood, and side effects alongside your meds. Great for chronic conditions like hypertension or depression. 4.6/5 on Google Play. Includes a visual timeline of your adherence over weeks and months.
- Round Health: Built for caregivers and families. Lets multiple people monitor a patient’s adherence. Ideal for elderly parents or loved ones with cognitive decline. Sends weekly reports to designated contacts.
- CareZone: More than just reminders. It’s a full medication organizer. Stores prescription info, pharmacy contacts, insurance details, and even tracks refills. Good for people juggling multiple doctors and pharmacies.
- Mango Health: Uses gamification. Earn points, unlock badges, and get gift cards for staying on track. Particularly effective for younger adults and those who respond to rewards.
These five apps account for over 60% of all downloads in the U.S. market. They’re not just popular-they’re proven. Studies show they improve adherence more than SMS reminders, pagers, or even motivational phone calls from nurses.
How They Help Specific Conditions
One-size-fits-all doesn’t work when it comes to meds. That’s why the most effective apps are becoming condition-specific.
For hypertension, apps like Medisafe and MyTherapy include blood pressure logging and alerts tied to medication timing. One study found patients using these apps reduced their systolic blood pressure by an average of 8 mmHg over six months-just by taking pills on time.
For diabetes, apps sync with glucose monitors. If your sugar drops too low after a missed insulin dose, the app flags it and reminds you to check your levels. Some even suggest adjustments based on food intake or activity.
For heart disease, apps like the Smart-Meds pilot program use storytelling and gamified narratives. Patients follow a character’s journey through recovery, making adherence feel less like a chore and more like part of a story they’re living.
Even for mental health meds-like antidepressants or antipsychotics-apps help by linking mood logs to dosing. You start to see patterns: “I felt worse after skipping my pill on Tuesday.” That kind of insight is powerful.
What You Need to Know Before You Download
These apps are powerful-but not magic. Here’s what actually matters when choosing one:
- Can you customize reminders? If you take pills at 7 a.m., 1 p.m., and 9 p.m., the app needs to handle multiple times per day, with different labels for each.
- Does it sync across devices? If you use an iPhone and an iPad, your data should follow you. Cloud sync is non-negotiable.
- Is it HIPAA-compliant? Your health data should be encrypted. Look for AES-256 encryption and TLS 1.2+ security. Most top apps meet this.
- Can someone else monitor you? For seniors or those with memory issues, letting a family member get alerts if you miss a dose can be lifesaving.
- Does it work offline? If you’re in a basement apartment with spotty Wi-Fi, the app still needs to function. Good apps save data locally and sync when you’re back online.
Also, don’t ignore the learning curve. A 2023 NIH study found that medically underserved patients needed about 22 minutes to set up Medisafe for the first time. But after a single 15-minute training session, 87% could use it alone. It’s not hard-it just takes a little help at first.
The Real Barriers-And How to Beat Them
Yes, apps work. But not everyone uses them. Why?
Older adults often say they’re “not tech-savvy.” But data shows otherwise. In federally qualified health centers, seniors using Medisafe had a 43% improvement in adherence-higher than younger users. The problem isn’t ability. It’s access. Many don’t own smartphones. Others can’t afford data plans. And some are scared to ask for help.
Low-income patients face the same issues. A 2024 survey found only 29% of adults over 65 use these apps, compared to 68% of those under 50. That’s a gap we can’t ignore.
Then there’s the tech itself. Battery drain. Missed notifications. Apps that stop updating. A 2025 Reddit thread showed 23% of iOS users complained about battery life. 31% of Android users reported missed alerts. These aren’t bugs-they’re dealbreakers.
Here’s how to fix it:
- Turn on “High Priority” notifications in your phone settings.
- Disable battery optimization for your app (Android: Settings > Apps > [App Name] > Battery > Don’t optimize).
- Use a second device if you’re worried-like a cheap Android tablet left on the nightstand.
- Pair the app with a smart pill dispenser (like Hero or AdhereTech) if you’re serious about reliability.
The Future: AI, Smart Bottles, and Real-Time Help
These apps aren’t staying the same. They’re getting smarter.
Medisafe’s June 2025 update now uses AI to predict when you’ll miss a dose-not just based on time, but on your mood logs, sleep patterns, and even weather (yes, some studies show rain correlates with missed meds). It then sends a tailored message: “You skipped your pill last time you felt tired. Want to take it now?”
By 2027, experts predict 35% of apps will connect to smart pill bottles. These bottles track when opened, send alerts to your phone, and even notify your pharmacist if you haven’t refilled. One study showed a 52% drop in missed doses when patients used smart bottles + app.
And reimbursement is changing. Health systems are starting to pay for these tools. If your app proves you’re taking your meds (and staying out of the ER), your insurer might cover it. Rock Health found apps with clear clinical results are 3.2 times more likely to get paid for.
Getting Started: Your 5-Minute Action Plan
Don’t wait. Start today.
- Choose one app: Medisafe or MyTherapy are the safest bets for beginners.
- Download it on your phone (iOS or Android).
- Open it and add your first medication. Take a photo of the pill bottle if you can.
- Set your first reminder. Make it 15 minutes before your usual time.
- Ask a family member or friend to help you set up the “Share with Caregiver” feature if you need it.
Do this now. Not tomorrow. Not next week. Right now. Your health depends on it.
What If the App Doesn’t Work for You?
Not every app fits every person. If you’ve tried one and it didn’t stick:
- Try a different one. MyTherapy’s interface is calmer than Medisafe’s. Round Health is better for families.
- Use it with a pill organizer. A simple seven-day box with morning/afternoon/evening slots can be paired with an app for extra backup.
- Ask your pharmacist. Many now offer free app setup sessions. They’ll walk you through it.
- Call your doctor. Some clinics now prescribe digital adherence tools as part of your care plan.
There’s no shame in switching. What matters is that you’re taking your meds-not which tool you use to do it.
Do medication reminder apps really work?
Yes, when used consistently. Studies show patients using apps like Medisafe and MyTherapy are twice as likely to take their meds as prescribed. Meta-analyses confirm they improve adherence more than alarms, SMS reminders, or even some counseling methods. Effect sizes are strong-Cohen’s d = 0.40-making them among the most effective tools available.
Are these apps safe and private?
Top apps like Medisafe, MyTherapy, and CareZone follow HIPAA standards. They use AES-256 encryption for stored data and TLS 1.2+ for data in transit. Your information isn’t shared with third parties unless you opt in. Always check the app’s privacy policy before entering health details.
Can older adults use these apps?
Absolutely. A 2023 NIH study found seniors in underserved communities improved adherence by 43% using Medisafe-even with no prior tech experience. The key is support: a 15-minute training session helped 87% of them use the app independently. Many apps also offer voice reminders and large buttons for easier use.
What if I miss a dose? Will the app punish me?
No. Good apps don’t judge-they help. Instead of shaming you, they’ll ask, “Want to take it now?” or “Was there a reason you missed it?” Some even let you log why you skipped, helping you and your doctor spot patterns. The goal is understanding, not guilt.
Do I need a smartphone to use these apps?
Yes, currently. All major apps require iOS 13+ or Android 8+. But if you don’t have a smartphone, talk to your pharmacist or doctor. Some clinics offer loaner devices or use low-tech alternatives like automated phone calls or smart pill dispensers that don’t need a phone.
Can my doctor see what I’m taking?
Only if you share it. Most apps let you export reports or send summaries to your provider via email or secure portal. Some, like Medisafe, integrate with electronic health records through FHIR APIs-but only if your clinic uses compatible systems and you give permission.
If you’re taking meds for a chronic condition, you’re already doing the hard part. The reminder app? That’s just the tool that makes it stick. No magic. No hype. Just better, simpler, smarter care.


Sachin Agnihotri
November 29, 2025 AT 22:08Man, I’ve been using Medisafe for my blood pressure meds, and it’s been a game-changer. I used to forget half the time, now I’m at 98% adherence. The photo feature? Genius. I just snap a pic of my pills and boom-no more guessing if it’s the blue one or the white one. Also, the family sync saved my dad’s life when he missed three doses in a row and my sister got alerted. Tech isn’t scary-it’s just medicine with a UI.
Diana Askew
December 1, 2025 AT 04:09These apps are just a gateway. 😏 The real agenda? Big Pharma + Silicon Valley are collecting your health data to sell to insurers so they can raise your premiums when you ‘fail’ adherence. They don’t care if you take your pills-they care if you’re ‘compliant’ enough to justify cutting your benefits later. I’ve seen the fine print. You’re not being helped-you’re being profiled. 🤖💊
King Property
December 2, 2025 AT 21:57Wow. Another feel-good tech article. Let me guess-you think downloading an app is the solution to systemic healthcare failure? 😂 You’re missing the point. Most people can’t afford their meds. No app fixes that. If your insulin costs $300/month, your ‘gamified rewards’ are meaningless. This isn’t about reminders-it’s about price gouging. And you’re selling Band-Aids while the patient bleeds out. Pathetic.
Yash Hemrajani
December 3, 2025 AT 08:29Let’s be real-apps work only if you’re not living in a basement with a 2012 Android and a 5% battery. 😅 I’ve seen grandmas try Medisafe, and they get stuck on the ‘add pill’ screen for 20 minutes. The real MVP? The pharmacist who sits down with you, holds your hand, and says, ‘Here, let me show you.’ No app replaces human patience. But hey, if you wanna feel tech-savvy while your uncle still uses a paper calendar? Go for it.
Pawittar Singh
December 3, 2025 AT 08:59Y’all are overthinking this. 🙌 I’m 68, never owned a smartphone till last year, and now I use MyTherapy with my granddaughter’s help. She set it up in 10 minutes. I get a voice reminder: ‘Pawittar, take your heart pill.’ I tap ‘yes’ and it chimes like a little victory bell. 🎉 No stress. No guilt. Just me, my meds, and a dumb app that doesn’t judge. If you’re still saying ‘I’m not techy,’ you’re just scared to ask for help. We’ve all been there. You got this.
Josh Evans
December 4, 2025 AT 06:53Just wanted to add-I use CareZone and it’s wild how much it organizes everything. I’ve got 7 meds, 3 pharmacies, and 2 doctors. Before, I had a shoebox full of papers. Now, I just open the app, see who needs a refill, and click ‘send request.’ It even tells me if my insurance approved it. Took me 3 days to learn it, but now I don’t know how I lived without it. Seriously, try it.
Allison Reed
December 5, 2025 AT 07:51This is exactly the kind of practical, compassionate health innovation we need. Apps like these don’t just improve adherence-they restore dignity. When you’re managing chronic illness, feeling in control matters as much as the medicine itself. Thank you for highlighting the human side of technology. This isn’t just data-it’s lives being changed, one reminder at a time.
Jacob Keil
December 5, 2025 AT 09:36ai predicts when you’ll miss a dose?? lol. you think your phone knows your soul? you think the weather affects your willpower? nah. it’s just math on a screen. and you’re letting it make you feel guilty for being human. we’re not machines. we’re messy. we’re tired. we’re scared. apps won’t fix that. they’ll just make you feel worse for not being perfect. 🤷♂️
Rosy Wilkens
December 5, 2025 AT 16:02Let me be clear: these apps are a Trojan horse. They’re not designed to help you-they’re designed to collect your biometric data, feed it to insurers, and then deny you coverage when you have a ‘poor adherence score.’ The FDA doesn’t regulate these. No one audits their algorithms. And yet, doctors are prescribing them? This isn’t healthcare. It’s surveillance capitalism with a pillbox interface. Wake up.
Andrea Jones
December 7, 2025 AT 02:11Okay but-has anyone tried pairing Mango Health with a dumb phone? I gave my mom an old iPhone I wasn’t using, turned off everything except the app, and now she gets her rewards and a little ‘you’re killing it!’ notification every week. She’s earned a Starbucks gift card. She says it’s the first thing she looks for in the morning. 🎯 I cried. Not because it’s tech. Because it made her feel proud. That’s worth more than any study.
Justina Maynard
December 8, 2025 AT 04:26I’ve been using Round Health for my dad with dementia. The weekly reports? I get them every Monday at 7 a.m. like a digital progress report. One week it said: ‘No doses missed for 14 days.’ I printed it out and taped it to the fridge. He saw it. He smiled. He said, ‘Did I do that?’ I said, ‘Yeah, pops. You did.’ No app can replace love-but this? This lets love show up when you can’t be there.
Evelyn Salazar Garcia
December 9, 2025 AT 03:17Why are we even talking about apps? Just give people free meds. Problem solved.