When your skin breaks out in thick, red, scaly patches, it’s easy to think it’s just a cosmetic issue. But for nearly one in three people with psoriasis, that’s only the beginning. Behind those flaky plaques lies a deeper, more dangerous problem: psoriatic arthritis. This isn’t just a skin condition or a joint problem-it’s both, at the same time, driven by the same faulty immune response. And if left unchecked, it can lead to permanent joint damage, chronic pain, and serious health risks beyond the skin.
What Exactly Is Psoriatic Arthritis?
Psoriatic arthritis (PsA) is an autoimmune disease where your immune system turns against your own body. Instead of fighting off germs, it attacks healthy tissues-especially the joints and the skin. About 30% of people with psoriasis will develop PsA, according to the American College of Rheumatology’s 2022 guidelines. For most, the skin comes first: about 85% of patients notice scaly patches on their elbows, knees, or scalp years before their joints start to hurt. But in 5 to 10% of cases, the joints swell and ache before any skin symptoms appear, making diagnosis trickier. The hallmark of PsA isn’t just joint pain. It’s inflammation in places you might not expect. You might notice your fingers or toes swelling up like sausages-that’s called dactylitis, and it affects nearly 40% of people with PsA. Or you might feel sharp pain at the bottom of your foot or behind your heel, where tendons attach to bone. That’s enthesitis, present in over a third of patients. These aren’t random symptoms. They’re clues pointing to a systemic autoimmune problem.How Doctors Diagnose Psoriatic Arthritis
There’s no single blood test that confirms PsA. Diagnosis relies on connecting the dots. Doctors use the CASPAR criteria, a set of rules established in 2006 that’s still the gold standard today. To meet the criteria, you need inflammatory joint disease plus at least three points from these categories:- Current or past psoriasis (3 points)
- Psoriatic nail changes like pitting or separation (1 point)
- Negative rheumatoid factor (1 point-this helps rule out rheumatoid arthritis)
- Characteristic bone changes on X-ray (1 point)
The Skin and Joint Connection
Psoriasis and PsA don’t just happen together-they’re two sides of the same coin. About 80 to 90% of PsA patients have the classic skin plaques: raised, red, silvery-scaled patches. But nail changes are even more telling. Eight out of ten people with PsA have pitted, thickened, or crumbling nails. That’s more common than joint swelling in some cases. The reason? The same immune cells-T-cells and cytokines like TNF-alpha and IL-17-are attacking your skin and your joints. These inflammatory signals travel through your bloodstream, triggering damage wherever they land. That’s why treating the skin alone won’t stop joint damage. You need to calm the immune system system-wide.
What Happens If It’s Not Treated
PsA doesn’t just cause discomfort-it causes destruction. Around 60 to 70% of patients with established disease show bone erosion on imaging. Without treatment, those small erosions grow. Joints can become misshapen. Mobility declines. Some people end up needing joint replacements. But the damage isn’t just in the joints. PsA is linked to a host of serious health problems. About half of people with PsA have metabolic syndrome-high blood pressure, high blood sugar, excess belly fat, and abnormal cholesterol. That raises heart attack risk by 43% compared to the general population. Depression and anxiety affect 20 to 30% of patients. Studies show their quality of life scores are 30 to 40% lower than people their age without the disease. And the numbers are grim: mortality in PsA patients is 30 to 50% higher than in the general population. The main cause? Heart disease. That’s why managing PsA isn’t just about pain relief-it’s about saving your life.How It’s Treated Today
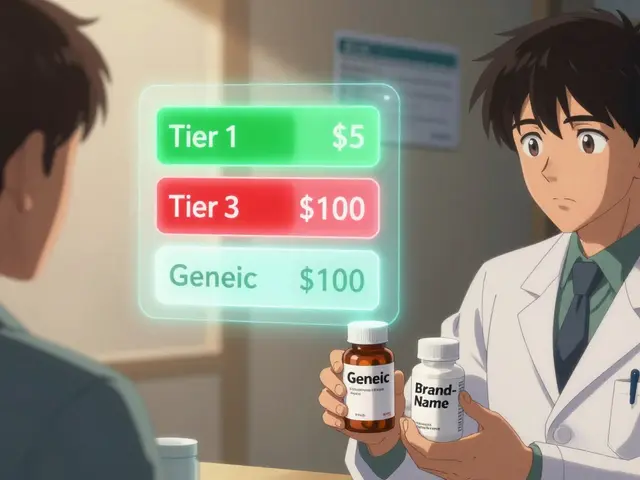
Treatment has changed dramatically in the last 15 years. In the past, doctors started with painkillers and anti-inflammatories like ibuprofen. Those help with mild symptoms, but they don’t stop joint damage. Now, treatment follows a step-up approach based on severity:- Mild cases: NSAIDs for pain and swelling.
- Moderate to severe: Methotrexate or other DMARDs to slow disease progression.
- Active disease with joint or skin involvement: Biologics or targeted drugs.
- IL-17 inhibitors (secukinumab, ixekizumab) are especially strong for skin clearance.
- IL-12/23 blockers (ustekinumab) help both skin and joints.
- JAK inhibitors like tofacitinib work inside cells to block inflammation signals.

What’s on the Horizon
Research is moving fast. Scientists are now looking at the gut-skin-joint axis. Early studies show people with PsA have different gut bacteria than healthy people. Could probiotics or dietary changes help? Clinical trials are testing that. New drugs are in the pipeline. Guselkumab and risankizumab target IL-23, a key driver of inflammation. Deucravacitinib, a TYK2 inhibitor, is already approved and shows promise with fewer side effects than older JAK drugs. Bimekizumab, which blocks both IL-17A and IL-17F, is showing even stronger results in trials. Advanced imaging is helping too. High-res ultrasound and MRI can now spot inflammation in tendons and joints before it causes pain. That means doctors can start treatment earlier-before irreversible damage happens.What You Can Do Now
If you have psoriasis and notice new joint stiffness, swelling, or pain-especially in your fingers, toes, or lower back-don’t wait. See a rheumatologist. Early treatment can prevent permanent damage. Lifestyle matters too. Losing weight reduces joint stress and lowers inflammation. Quitting smoking cuts your risk of heart disease. Regular exercise keeps joints flexible and helps manage depression. And don’t ignore your mental health. Counseling and support groups can make a real difference in how you cope. The National Psoriasis Foundation’s 2025 Pocket Guide defines moderate disease as 3 to 10% of your skin covered in plaques. Severe is over 10%. But numbers don’t tell the whole story. If your joints hurt, your nails are crumbling, or you’re too tired to get out of bed, you’re not just “a little inflamed.” You need a full plan.Final Thoughts
Psoriasis and psoriatic arthritis aren’t just skin-deep. They’re signs your immune system is on fire. The good news? We have more tools than ever to put that fire out. The bad news? Many people still wait too long to get help. You don’t have to live with constant pain. You don’t have to accept joint damage as inevitable. With the right diagnosis and treatment, most people with PsA can reach minimal disease activity-and live full, active lives. The key is acting before the damage becomes permanent.Can psoriasis turn into psoriatic arthritis?
Yes, but not everyone with psoriasis develops psoriatic arthritis. About 30% of people with psoriasis will go on to develop joint symptoms. For most, the skin condition comes first, often years before the joints are affected. In a small number of cases, joint pain appears before any skin changes.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. While both are autoimmune joint diseases, they’re different. Rheumatoid arthritis usually affects the same joints on both sides of the body and tests positive for rheumatoid factor. Psoriatic arthritis often affects joints asymmetrically, causes dactylitis (sausage fingers), and is linked to psoriasis and nail changes. Blood tests for rheumatoid factor are typically negative in PsA.
Can psoriatic arthritis be cured?
There’s no cure yet, but it can be controlled. With the right treatment, most people can reach minimal disease activity-meaning little to no pain, swelling, or skin involvement. Early treatment is critical to prevent permanent joint damage. Many patients live full, active lives with proper management.
What triggers psoriatic arthritis flares?
Common triggers include stress, infections (like strep throat), injury to the skin or joints, smoking, heavy alcohol use, and being overweight. Some people notice flares after stopping medication too quickly. Identifying your personal triggers and avoiding them helps keep symptoms under control.
Does psoriatic arthritis affect life expectancy?
Yes, studies show people with PsA have a 30 to 50% higher risk of early death compared to the general population, mostly due to heart disease. This is why managing PsA isn’t just about joints-it’s about overall health. Controlling inflammation, losing weight, quitting smoking, and monitoring blood pressure and cholesterol are just as important as taking your medication.
Are biologics safe for long-term use?
Biologics are generally safe for long-term use, but they do carry risks. Because they suppress parts of the immune system, they can increase the chance of serious infections like tuberculosis or fungal infections. Before starting, you’ll be screened for latent TB and hepatitis. Regular monitoring and reporting any fever, chills, or unusual fatigue are critical. The benefits of preventing joint damage and improving quality of life usually outweigh the risks.


Jenny Lee
November 18, 2025 AT 20:15Just got diagnosed last month. My nails have been crumbling for years-I thought it was just dry skin. Turns out, it was PsA. I’m on secukinumab now. Skin’s clear. Joints don’t scream at 5 a.m. Life changed.
Evan Brady
November 20, 2025 AT 07:30For real-most people think psoriasis is just ‘bad eczema.’ Nope. It’s systemic inflammation wearing a skin suit. If your joints hurt, even a little, don’t wait. Get an MRI. Early intervention saves tendons, not just dignity.
Brandon Lowi
November 21, 2025 AT 22:45Look, I’m American, and I’ve seen the medical-industrial complex turn a simple skin rash into a $20,000-a-year biologic nightmare. But here’s the truth: if you’re not treating the immune system, you’re just putting a bandage on a hemorrhage. Biologics? They’re not a scam-they’re science. Stop listening to TikTok ‘naturopaths’.
Ancel Fortuin
November 23, 2025 AT 12:33They say ‘early treatment saves joints’-but who’s really funding these studies? Big Pharma? The same companies that made opioids? I’ve got a cousin who got on a biologic… now he’s got shingles, a fungal lung infection, and a $12,000 co-pay. They’re selling hope like it’s a subscription box.
Shravan Jain
November 23, 2025 AT 20:41One must acknowledge the ontological dissonance between the phenomenological experience of cutaneous eruption and the systemic immunological cascade. The epidermal manifestation is but a semiotic surface, a mere symptomatum of a deeper, more insidious autoimmune ontogeny. One cannot treat the epidermis without addressing the cytokine architecture beneath. Hence, the therapeutic imperative is not local, but cosmological.
Jeff Hakojarvi
November 24, 2025 AT 16:41I’m a nurse who’s seen this play out 200 times. People wait until their fingers look like sausages and their spine feels like concrete. Don’t be that person. Go to a rheumatologist. Bring your skin photos. Ask for an ultrasound. It’s not ‘overreacting’-it’s being smart. You’re not weak for needing help. You’re brave for asking.
Ram tech
November 25, 2025 AT 08:1130% of psoriasis people get joint stuff? That’s low. I think it’s more like 70%. My uncle had it. His knees looked like old tires. He didn’t do anything till he couldn’t walk. Now he’s on disability. Don’t be him.
Hannah Blower
November 26, 2025 AT 18:45Let’s be honest: if you’re not on a biologic by your third flare, you’re being negligent. The data is clear. The guidelines are clear. The only thing holding people back is the delusion that ‘natural remedies’ can outsmart a cytokine storm. You don’t heal a war with chamomile tea.
Gregory Gonzalez
November 28, 2025 AT 12:40Oh, so now we’re supposed to believe that a 2006 diagnostic criteria is still ‘gold standard’? How quaint. The world moved on. We have AI-powered joint imaging, proteomic profiling, gut microbiome signatures… and we’re still counting nail pitting like it’s 2006? Progress is a myth peddled by academic gatekeepers.
mithun mohanta
November 28, 2025 AT 14:06Look. I’m not a doctor. But I read a paper once. And I know that IL-17 is the real villain. TNF is so… 2010. If you’re still on adalimumab, you’re basically using a flip phone while everyone else has an iPhone 16. Wake up. Your skin deserves better.
Ronald Stenger
November 28, 2025 AT 14:13They say ‘heart disease risk is 43% higher’-but they never mention that the NSAIDs they prescribe for pain are the real reason you’re having heart issues. It’s a trap. Take the drug, get heart damage. Don’t take the drug, get joint damage. Either way, you lose. Welcome to American medicine.
Alex Boozan
November 30, 2025 AT 01:26Let’s not conflate correlation with causation. The gut-skin-joint axis? That’s a hypothesis with 17 mouse studies and zero RCTs in humans. Meanwhile, we’re prescribing probiotics like they’re insulin. We’ve turned immunology into a cult of microbial dogma. The real villain? Chronic stress. Not IL-23. Not TNF. Not your microbiome. Your boss.
Timothy Uchechukwu
November 30, 2025 AT 06:45In my country we don't need biologics we just eat neem leaves and pray to ancestors and the psoriasis goes away. You westerners think medicine is pills and machines but we know the truth. Your joints hurt because you eat too much sugar and watch too much screen. Fix your soul not your immune system
Richard Couron
December 1, 2025 AT 15:43They’re lying about the mortality stats. The CDC hides the real numbers. The real cause of death? The biologics themselves. They’re not treating PsA-they’re turning you into a walking immunosuppressed lab rat. The government knows. The pharma knows. You don’t. But now you do.