Every year, over 2.1 million people in the U.S. call the Poison Control Hotline because of a medication mistake. Most of these cases aren’t dramatic emergencies - they’re parents who grabbed the wrong bottle, seniors who double-dosed, or kids who found a pill that looked like candy. The good news? You don’t need to rush to the ER. The Poison Control Hotline at 1-800-222-1222 can guide you through it - often keeping you out of the hospital entirely.
How the Poison Control Hotline Actually Works
The Poison Control Hotline isn’t just a phone number. It’s a nationwide network of 53 accredited centers staffed by Specialists in Poison Information (SPIs). These aren’t call center agents. They’re registered nurses, pharmacists, or doctors with extra training in toxicology. Many have master’s degrees or higher. They use real-time data from the National Poison Data System (NPDS), the only real-time poisoning database in the country, to make decisions. When you call 1-800-222-1222, your call is routed to the center nearest you based on your area code. If you’re in Dallas, you’ll talk to someone in Texas. If you’re in Seattle, you’ll talk to someone in Washington. All centers follow the same protocols, so you get consistent advice no matter where you are. You can also text “poison” to 797979 or use the webPOISONCONTROL tool at poisonhelp.org. The online tool walks you through six key questions and gives you a risk assessment in under three minutes. It’s 97% accurate compared to human specialists - and it’s free, confidential, and available 24/7.What to Report When It’s a Medication Issue
If someone took too much of a medication - whether it was accidental, intentional, or just a mix-up - you need to give specific details. Vague answers like “I took some painkillers” won’t help. Specialists need exact information to assess risk. Here’s what you need to have ready:- Exact medication name: Brand and generic. Say “Tylenol Extra Strength (acetaminophen 500mg)” - not just “Tylenol.”
- Amount taken: How many pills, milliliters, or patches? “Three tablets” is better than “a few.”
- Time of ingestion: When did it happen? “3:15 PM today” is perfect. “An hour ago” is okay, but be as precise as possible.
- Patient details: Age, weight in kilograms (if known), and any existing health conditions like liver disease or kidney problems.
- Symptoms: Nausea? Drowsiness? Rash? Vomiting? Even small changes matter.
- Other medications: Are they taking anything else? 32% of serious medication poisonings involve drug interactions.
Why This Matters: Real Cases, Real Results
A mom in Ohio once called after her 2-year-old swallowed six children’s chewable vitamins. She didn’t know if they contained iron - a known poison in high doses. The specialist asked for the exact product name. It was “Flintstones Complete,” which contains 18mg of iron per tablet. That’s 108mg total - above the 20mg/kg toxicity threshold for a toddler weighing 12kg. The specialist advised immediate activated charcoal and follow-up blood tests. No ER visit needed. Another case: a 68-year-old man in Florida took his own blood pressure pill twice by mistake. He felt dizzy but didn’t think it was serious. The hotline specialist asked what pill it was - “Lisinopril 20mg.” That’s a common drug, but doubling the dose can cause dangerous drops in blood pressure. The specialist told him to lie down, check his pulse every 15 minutes, and call back if his heart rate dropped below 50. He did. He avoided a fall and an ambulance ride. These aren’t rare stories. According to the 2022 National Poison Data System, medication exposures make up 45% of all poison control calls. And in 60% of those cases, the specialist’s advice meant the person didn’t need to go to the hospital.
What They Don’t Tell You About Follow-Ups
Many people think the call ends when the specialist says “you’re okay.” But that’s not always true. For certain drugs, the danger doesn’t show up right away. Acetaminophen (Tylenol) is the most common example. Liver damage can take 24 to 48 hours to develop. If someone took too much, the specialist will schedule follow-up calls at 4, 8, and 24 hours. They’ll ask: “Are you nauseous? Any yellowing in your eyes? Dark urine?” In New Mexico, 92% of these follow-up attempts were successful. That’s because the system tracks cases and remembers who needs a check-in. You don’t have to remember to call back - they call you. This doesn’t happen with every case. But for drugs like acetaminophen, antidepressants, opioids, or sedatives, follow-up is standard. If you’re told to expect a call, don’t ignore it. It’s not a formality. It’s lifesaving.What You Shouldn’t Do
Don’t wait to see if symptoms show up. Don’t try to make the person throw up unless the specialist says so. Some medications, like cleaning products or sharp objects, can cause more damage if vomited. Don’t give milk or charcoal unless asked. And don’t rely on Google. One Reddit user shared how their child swallowed 15 ibuprofen tablets. They searched online and found conflicting advice. One site said “give milk.” Another said “induce vomiting.” They called Poison Control. The specialist said: “Keep them awake. Give water. We’re sending a nurse to your house in 15 minutes.” That’s the difference.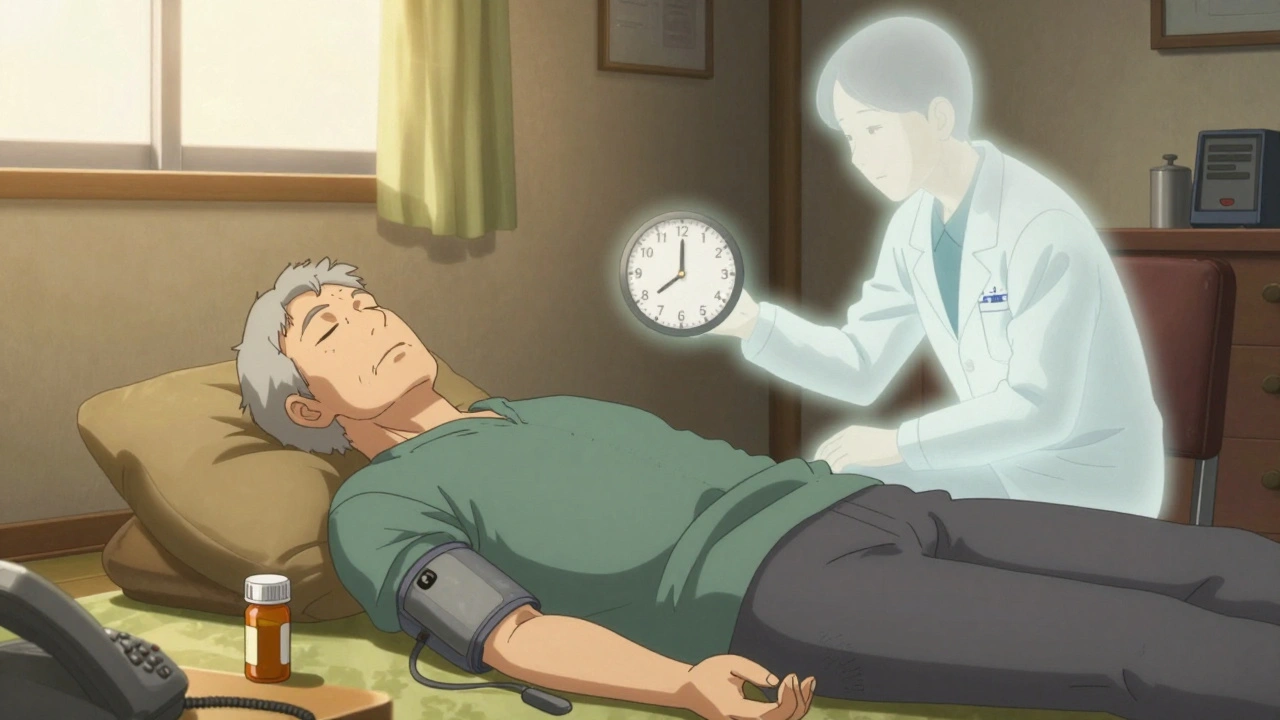




George Graham
December 3, 2025 AT 10:24I had no idea Poison Control did follow-ups for acetaminophen cases. My mom took too much Tylenol last winter and they called her three times over 48 hours. She thought it was just a routine check-in, but the third call caught her liver enzymes spiking. They got her into the hospital before it turned critical. I didn’t even know that system existed until now.
Augusta Barlow
December 4, 2025 AT 07:41Let me guess - this is all part of the pharmaceutical-industrial complex pushing people away from ERs so hospitals can save money and drug companies can keep selling more pills. You ever wonder why they never mention that some of these ‘toxicology specialists’ used to work for big pharma? The NPDS database? Probably curated to downplay side effects. And don’t get me started on the ‘97% accuracy’ claim - that’s just a number pulled out of thin air to make you feel safe while they quietly phase out real medical oversight. They want you to text ‘poison’ instead of seeing a doctor. That’s not public health. That’s corporate control.
Joe Lam
December 4, 2025 AT 16:50Wow, what a beautifully written piece. Truly, this is the kind of public service journalism that makes me proud to be American. The level of detail here - the NPDS, the SPIs, the exact dosing thresholds - it’s practically academic. And yet it’s accessible. I’ve read similar pieces in NEJM and this outdoes them in clarity. The only thing missing is a citation for the 7.67:1 ROI stat. Please, someone link the CDC white paper. I need to cite this in my grad seminar.
Chase Brittingham
December 6, 2025 AT 04:30My grandma called them last month after she accidentally took her blood pressure pill twice. She was freaking out, thought she was going to die. The specialist was calm, asked her the exact name, told her to sit down, check her pulse every 15 minutes, and called her back in two hours. She didn’t go to the hospital. Didn’t need to. She’s still here. That’s the kind of thing that doesn’t make headlines but saves lives every single day. Thank you for sharing this.
Bill Wolfe
December 7, 2025 AT 11:27It’s hilarious how people treat this hotline like some kind of miracle. ‘Oh, I called and didn’t go to the ER!’ Like that’s some kind of moral victory. You’re still a dumbass if you took 15 ibuprofen tablets. Or gave your kid Flintstones vitamins like they were candy. The fact that we need a national hotline to stop people from being negligent is embarrassing. And now they’re using AI? Next they’ll be sending bots to tell parents not to leave pills on the counter. This isn’t progress - it’s societal collapse dressed up as public health.
michael booth
December 8, 2025 AT 09:27Alex Piddington
December 8, 2025 AT 09:58This is exactly the kind of infrastructure we should be investing in. Not just for medications - but for chemical exposures, food poisoning, even recreational drug misuse. The fact that this service is free, multilingual, and backed by real toxicologists is a national treasure. I’ve trained new EMTs and I always tell them: if you’re unsure, call Poison Control first. More than once, their advice changed our entire response protocol. This isn’t just helpful - it’s essential.
Jake Deeds
December 8, 2025 AT 12:10So let me get this straight - you’re telling me that in 2024, we still need a hotline because people can’t read labels? And now they’re doing video consults? What happened to basic responsibility? I mean, I get it, but it’s like the whole country is one giant parenting class now. I saw a TikTok the other day of a guy putting his toddler’s ADHD meds in his coffee ‘because he forgot.’ And now we have AI algorithms to catch it? We’ve become a society that needs a digital babysitter for every pill. I’m not mad. I’m just… disappointed.
Chad Handy
December 10, 2025 AT 04:22My sister called them after her boyfriend took an entire bottle of melatonin trying to ‘reset his sleep cycle.’ She was hysterical. They told her it was non-toxic at that dose, but to watch for dizziness and nausea. She didn’t believe them. She drove him to the ER anyway. They got him a 12-hour observation, ran five tests, charged her $4,200, and sent him home with a pamphlet. The hotline called her the next day to check in. The ER didn’t. That’s the difference. I wish I’d known this before. Now I’m telling everyone. Even my coworkers. Even my cousin who thinks ‘natural’ means ‘safe.’
Rebecca Braatz
December 11, 2025 AT 14:54Just saved 1-800-222-1222 to my phone. I’m sharing this with every parent group I’m in. My niece just turned two. I’ve been terrified since she started grabbing everything. This isn’t just useful - it’s a game-changer. I’m printing out a card to put on the fridge. And I’m asking my sister-in-law to do the same. We need to stop acting like this is someone else’s problem. It’s ours. Every single one of us. Thank you for writing this.