Understanding Hepatic Encephalopathy and its Connection to the Central Nervous System
Hepatic encephalopathy is a complex neuropsychiatric syndrome that occurs as a result of acute or chronic liver failure. It is characterized by a wide range of cognitive, psychiatric, and motor disturbances, affecting the central nervous system (CNS). In this section, we will delve into the basics of hepatic encephalopathy and its impact on the CNS. We will also discuss the various factors that contribute to the development of this condition, as well as its clinical manifestations.
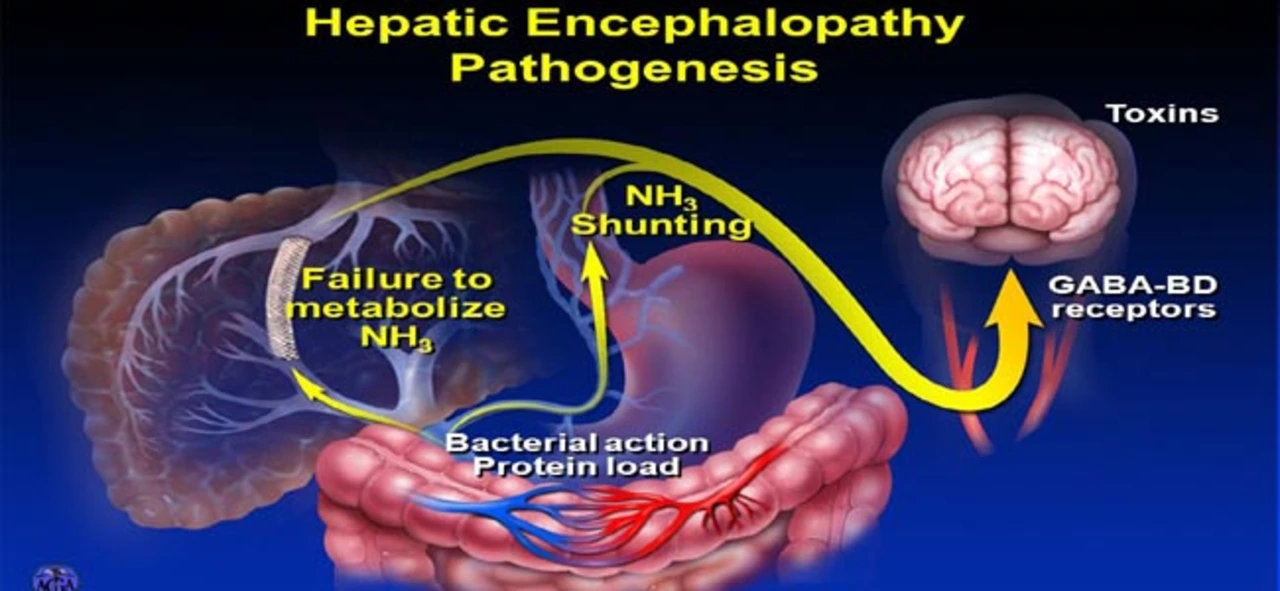
The Role of Ammonia in Hepatic Encephalopathy
One of the primary factors contributing to hepatic encephalopathy is the accumulation of ammonia in the blood. Under normal circumstances, ammonia is produced as a byproduct of protein metabolism and is effectively detoxified by the liver. However, in cases of liver dysfunction, ammonia levels can rise, leading to increased concentrations in the blood and brain. This impaired ammonia metabolism has been shown to play a significant role in the development of hepatic encephalopathy and the ensuing neurological complications, including brain edema and alterations in neurotransmission.
Neurotransmitter Imbalances and Hepatic Encephalopathy
Another key aspect of hepatic encephalopathy is the disruption of neurotransmitter balance within the CNS. The elevated ammonia levels associated with liver dysfunction can alter the levels of key neurotransmitters such as glutamate, gamma-aminobutyric acid (GABA), and serotonin. These imbalances can result in a variety of neurological symptoms, including cognitive impairment, mood disturbances, and motor dysfunction. Understanding the role of neurotransmitter imbalances in hepatic encephalopathy can provide valuable insights into potential treatment strategies for this complex condition.
Cognitive and Psychiatric Manifestations of Hepatic Encephalopathy
Patients with hepatic encephalopathy often exhibit a wide range of cognitive and psychiatric symptoms. These can include memory impairment, attention deficits, confusion, disorientation, and even coma in severe cases. Additionally, mood disturbances such as depression, anxiety, and irritability are common in patients with hepatic encephalopathy. The severity of these symptoms can vary greatly depending on the stage of the disease and the extent of liver dysfunction. Early detection and intervention are crucial in order to minimize the impact of hepatic encephalopathy on patients' cognitive and psychiatric well-being.
Motor Disturbances in Hepatic Encephalopathy
In addition to cognitive and psychiatric symptoms, hepatic encephalopathy can also cause a range of motor disturbances. These can include muscle stiffness, tremors, unsteady gait, and even seizures in some cases. The motor symptoms of hepatic encephalopathy are often closely linked to the neurotransmitter imbalances that occur within the CNS as a result of liver dysfunction. Addressing these imbalances through targeted therapeutic interventions can help to alleviate motor disturbances and improve patients' overall quality of life.
Treatment Approaches for Hepatic Encephalopathy
Given the complex nature of hepatic encephalopathy and its impact on the CNS, a multifaceted treatment approach is often required. This may include strategies aimed at reducing ammonia levels, such as the use of lactulose or rifaximin, as well as interventions targeting neurotransmitter imbalances. In addition, supportive care measures such as nutritional support, electrolyte management, and the treatment of underlying liver disease are essential components of the overall treatment plan. Early diagnosis and intervention are key to optimizing patient outcomes and minimizing the long-term impact of hepatic encephalopathy on the CNS.


Prema Amrita
June 2, 2023 AT 01:06It's not dementia. It's not stroke. It's liver failure whispering through your neurons.
Alex Rose
June 2, 2023 AT 11:07Vasudha Menia
June 2, 2023 AT 21:30It’s not just medical-it’s heartbreaking. But please, if you or someone you love has cirrhosis-don’t ignore the small signs. Confusion, slurred speech, sleepiness… don’t wait for coma. Early = better.
Love you all. 💙
Mim Scala
June 3, 2023 AT 08:41Bryan Heathcote
June 3, 2023 AT 12:55