Endometriosis Symptom Checker
Symptom Assessment
Answer the following questions to assess your risk for endometriosis. This tool is for educational purposes only and does not replace professional medical advice.
Assessment Result
When it comes to women’s health, pelvic exam is a hands‑on clinical assessment that evaluates the reproductive organs for abnormalities that can flag serious conditions early. One of the most common, yet often missed, conditions is endometriosis-a disease that affects roughly 1 in 10 women of reproductive age. The exam isn’t a magic detector, but it’s the first line of defense that can point doctors toward deeper testing before pain escalates.
Quick Takeaways
- A pelvic exam can reveal tenderness, nodules, or irregularities linked to endometriosis.
- Typical signs include painful periods, deep pelvic pain, and pain during intercourse.
- The exam is quick, usually 5‑10 minutes, and can be done in a regular office visit.
- If the exam suggests endometriosis, doctors often follow up with ultrasound or laparoscopy.
- Preparing mentally and physically helps the exam feel less intimidating.
What Exactly Is a Pelvic Exam?
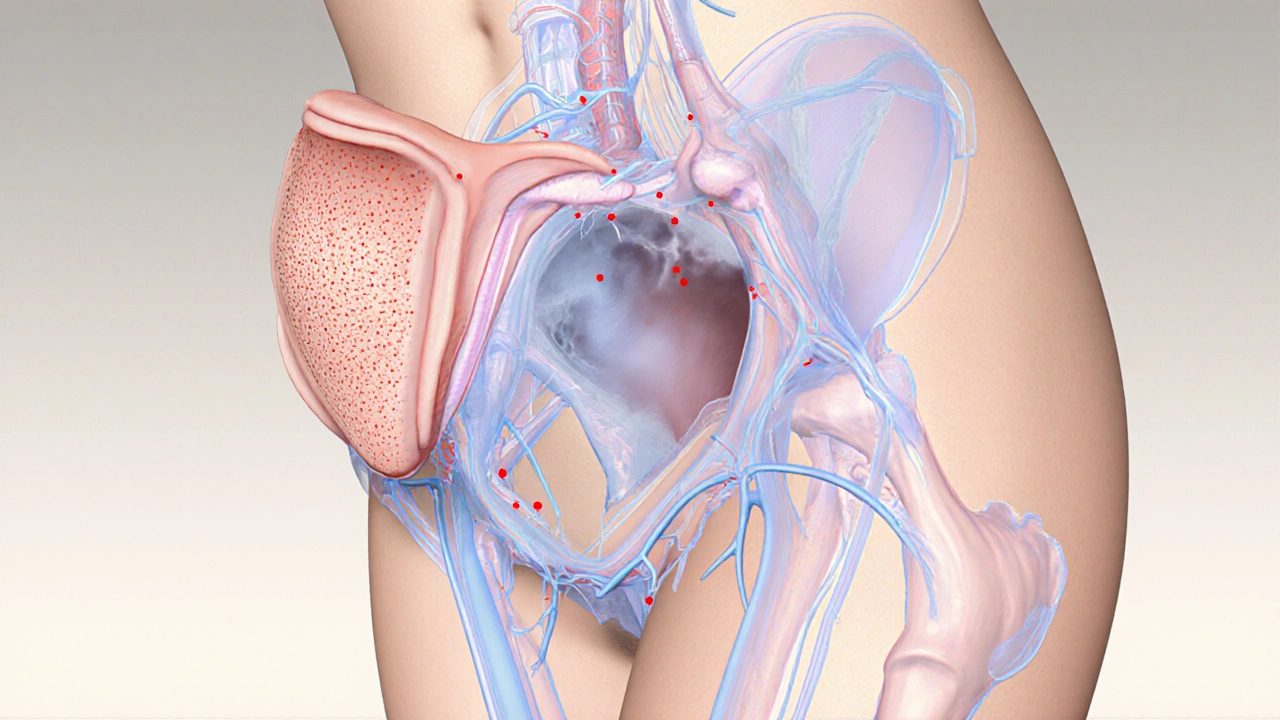
The exam consists of two parts: an external visual inspection and an internal manual assessment. First, the clinician checks the vulva, labia, and surrounding skin for lesions, discharge, or swelling. Then, using a gloved hand and a speculum, they feel the uterus, ovaries, and the spaces around them (the pouch of Douglas) for size, position, and any irregular masses.
During the internal portion, the doctor may ask you to squeeze your pelvic floor muscles or change breath patterns. These cues help differentiate normal tenderness from the deep, constant ache that often signals endometriosis implants.
Key Endometriosis Signs a Pelvic Exam Can Spot
While definitive diagnosis usually needs imaging or surgery, a skilled Gynecologist a medical doctor specializing in female reproductive health can pick up several red flags:
- Tender nodules on the uterosacral ligaments-small, rope‑like structures that support the uterus.
- Enlarged, fixed ovaries that feel “sticky” rather than mobile.
- Deep tenderness in the pouch of Douglas, which often correlates with posterior implants.
- Visible adhesions or scar tissue during the speculum view, though these are rare without advanced disease.
These findings don’t confirm endometriosis, but they give the doctor a strong suspicion that warrants further testing.
How the Exam Fits Into the Full Diagnostic Path
Think of the pelvic exam as the first puzzle piece. If something looks off, doctors usually order a transvaginal Ultrasound an imaging technique that uses high‑frequency sound waves to create pictures of pelvic organs. Ultrasound can spot ovarian endometriomas (the classic “chocolate cysts”) and large implants on the uterine surface.
When ultrasound is inconclusive, the gold‑standard test is Laparoscopy a minimally invasive surgical procedure that lets doctors view and biopsy the pelvic cavity. Laparoscopy not only confirms the diagnosis but also allows immediate removal of visible lesions.
Below is a quick side‑by‑side look at the three main tools.
| Tool | Invasiveness | What It Detects | Typical Use |
|---|---|---|---|
| Pelvic Exam | Non‑invasive | Tenderness, nodules, fixed ovaries | First‑line screening |
| Transvaginal Ultrasound | Non‑invasive | Ovarian endometriomas, deep infiltrating lesions | Follow‑up imaging |
| Laparoscopy | Minimally invasive surgery | All lesion types, histological confirmation | Definitive diagnosis & treatment |
Preparing for Your Pelvic Exam
Many women avoid the exam because it feels vulnerable. A few practical steps can make it smoother:
- Schedule the appointment during the early follicular phase (days 5‑10 of your cycle) when the uterus is less likely to be enlarged.
- Empty your bladder beforehand; a full bladder can make the exam uncomfortable.
- Wear a simple, cotton underwear and bring a change of clothes if you prefer.
- Write down any symptoms-pain timing, intensity, menstrual irregularities-so you don’t forget them.
- Ask the clinician to explain each step before they start; transparency reduces anxiety.
What to Do After an Abnormal Finding
If the doctor notes suspicious signs, they’ll likely recommend one of the following pathways:
- Imaging: A targeted ultrasound or MRI can map deeper lesions that are hard to feel.
- Medical management: Hormonal therapy (combined oral contraceptives, progestins, GnRH agonists) can shrink lesions and relieve pain while you await imaging.
- Surgical referral: For severe pain or infertility concerns, a referral to a laparoscopic surgeon is common.
Throughout this process, keep a symptom diary. Tracking pain scores, menstrual flow, and any changes after treatment helps the medical team fine‑tune the plan.
Common Myths About Pelvic Exams and Endometriosis
Myth #1: “If the exam is normal, I don’t have endometriosis.” False. Early disease can hide from touch, especially deep implants outside the reachable area.
Myth #2: “The exam will be painful.” Most clinicians use a gentle technique; you can request a break at any time.
Myth #3: “Only severe pain means endometriosis.” Many women experience mild, chronic discomfort that still impacts quality of life.
When to Seek Help
Don’t wait for pain to become unbearable. Consider an appointment if you notice any of these patterns:
- Menstrual cramps that last more than 3‑4 days.
- Pain during or after sex (dyspareunia).
- Unexplained fatigue or gastrointestinal upset that syncs with your cycle.
- Difficulty conceiving after trying for six months.
Early evaluation can shave years off the diagnostic journey, which, according to a 2023 Guttmacher Institute report, averages 7‑10 years for most patients.
Bottom Line
A well‑performed pelvic exam is a low‑cost, low‑risk tool that can set the diagnostic chain in motion for endometriosis. While it won’t replace imaging or surgery, it gives your gynecologist a crucial clue about where to look next. Pair the exam with clear symptom reporting, timely follow‑up imaging, and, when needed, minimally invasive surgery, and you’ll be on a faster path to relief.
Frequently Asked Questions
Can a pelvic exam diagnose endometriosis on its own?
No. The exam can raise suspicion by finding tenderness or nodules, but definitive diagnosis usually requires imaging or laparoscopic biopsy.
How often should I get a pelvic exam if I have endometriosis symptoms?
If you have persistent or worsening symptoms, an annual exam is advisable. Your doctor may suggest more frequent checks if treatment changes or new pain patterns emerge.
Is the pelvic exam painful for women with endometriosis?
It can be uncomfortable because the disease often makes pelvic tissues extra sensitive. Communicating with your clinician about pain levels helps them adjust pressure and technique.
What other conditions can mimic endometriosis during a pelvic exam?
Pelvic inflammatory disease, ovarian cysts, fibroids, and adhesions from prior surgeries can produce similar tenderness or palpable masses.
Can I request a specific type of exam (e.g., speculum‑free) if I’m anxious?
Yes. Many clinics offer a “no‑speculum” exam that focuses on external and bimanual assessment. Discuss your comfort level with the provider before the visit.





William Goodwin
October 2, 2025 AT 20:36Hey folks, let’s celebrate how a simple pelvic exam can be a game‑changer for women worldwide 🌍✨. It’s not just a medical routine; it’s a bridge between hidden pain and relief, and that’s something we all can rally behind. Think of it as a cultural checkpoint, reminding us that health equity starts with open conversations. If you’ve ever felt the silence around endometriosis, know that this exam is a doorway to being heard. 🙌💙
Isha Bansal
October 4, 2025 AT 00:23It is incumbent upon us to observe the precise terminology when discussing gynecological assessments, for the integrity of medical discourse hinges upon linguistic exactitude. The phrase ’pelvic exam’ must be rendered without colloquial abbreviation, and the term ’endometriosis’ should never be misspelled or trivialized, lest we undermine the gravitas of the condition. Moreover, the discourse should reflect the pioneering strides of our own nation’s researchers, whose contributions to reproductive health deserve recognition alongside Western counterparts. One must also note that the diagnostic pathway, as delineated, follows a hierarchical protocol that is universally applicable, yet the cultural context of patient comfort varies markedly across regions. It is therefore essential to adopt a lexicon that respects both scientific rigor and the diverse sociocultural fabric of our nation, thereby fostering a more inclusive narrative. In sum, let us refrain from imprecise language, for precision is the hallmark of both national pride and medical excellence.
Ken Elelegwu
October 5, 2025 AT 04:09One might posit that the pelvic examination represents a subtle art, a careful choreography between clinician and patient, wherein the subtleties of tissue tension reveal the unseen. The discerning practitioner, much like a connoisseur of fine literature, discerns the faintest nodules as one would a hidden metaphor within a sonnet. Yet, let us not be austere; the process is fundamentally about alleviation of suffering, a noble pursuit that bridges the empirical and the humane. In this light, the exam is both a diagnostic instrument and an emblem of compassionate inquiry.
Gene Nilsson
October 6, 2025 AT 07:56It is of utmost importance that patients understand the non‑invasive nature of the pelvic exam, as it serves as the first line of defense against potential pathologies. The clinician should elucidate each step, ensuring that the individual feels both respected and at ease. Unfortunately, many individuals remain misinformed, which may lead to undue anxiety; thus, clarity in communication is paramount. Its vital that we address these concerns with both scientific rigour and empathetic outreach.
Anshul Gupta
October 7, 2025 AT 11:43Honestly, most of this sounds like textbook fluff that doesn’t help anyone in the real world.
Maryanne robinson
October 8, 2025 AT 15:29Let’s break down why a pelvic exam can be such a pivotal step on the road to diagnosing endometriosis, and I’ll walk you through each component with as much clarity as possible. First, the exam offers a direct, hands‑on assessment that can uncover tenderness or nodules that imaging might miss, especially in the early stages of the disease. Second, it provides an immediate opportunity for the clinician to ask detailed, targeted questions about your menstrual cycle, pain patterns, and any fertility concerns, which are essential data points for constructing a diagnostic hypothesis. Third, the comfort of the patient is paramount; scheduling the appointment during the early follicular phase typically reduces uterine size and makes the exam less uncomfortable, a practical tip that many overlook. Fourth, after an abnormal finding, the physician can promptly arrange a transvaginal ultrasound, which visualizes ovarian endometriomas-those classic “chocolate cysts” that are hallmark lesions. Fifth, in cases where ultrasound results are inconclusive, the doctor may recommend laparoscopy, the gold‑standard that not only confirms the diagnosis but also allows for immediate lesion removal. Sixth, it’s crucial to keep a symptom diary, noting pain intensity on a scale of 1‑10, timing relative to your cycle, and any triggers; this diary becomes a powerful communication tool during follow‑up visits. Seventh, don’t underestimate the psychological impact-knowing that a professional is actively investigating the cause of your pain can alleviate anxiety, which in turn can lower perceived pain levels. Eighth, the exam is relatively quick, often completed within five to ten minutes, making it a low‑cost, low‑risk entry point into a comprehensive diagnostic algorithm. Ninth, many clinicians now offer “no‑speculum” options for those with heightened anxiety, focusing on external and bimanual assessment, which maintains diagnostic value while respecting patient comfort. Tenth, being proactive and advocating for yourself-asking the doctor to explain each step and voicing any concerns-can dramatically improve the thoroughness of the exam. Eleventh, if you receive reassurance that the exam is normal, remember that early disease can sometimes evade detection, so persistent symptoms should still prompt further evaluation. Twelfth, hormonal therapies such as combined oral contraceptives or GnRH agonists can be initiated while awaiting imaging, providing symptomatic relief in the interim. Thirteenth, multidisciplinary care involving pain specialists, fertility experts, and mental health professionals can optimize outcomes for complex cases. Fourteenth, education is power; familiarizing yourself with the anatomy of the uterosacral ligaments and the pouch of Douglas helps you understand why certain findings are significant. Fifteenth, community support groups can offer shared experiences that validate your journey and provide practical tips for navigating appointments. Finally, early and consistent engagement with your healthcare provider, anchored by that initial pelvic exam, can shave years off the typical diagnostic odyssey, delivering faster relief and better quality of life.
Erika Ponce
October 9, 2025 AT 19:16Understanding that a quick exam can spot early warning signs is reassuring, and keeping track of symptoms makes the whole process smoother for everyone involved.
Danny de Zayas
October 10, 2025 AT 23:03Sounds like a solid first step.
John Vallee
October 12, 2025 AT 02:49Indeed, the brevity of the statement captures the essence, but let’s not forget that clear communication about each step of the exam can empower patients and improve outcomes.
Brian Davis
October 13, 2025 AT 06:36Adding to that, many cultures view pelvic health as a private matter, so framing the exam as a respectful, collaborative dialogue can bridge cultural gaps while preserving the clinical thoroughness you highlighted.
jenni williams
October 14, 2025 AT 10:23Hey there, I totally get how overwhelming this can feel, but remember you’re not alone in this journey 😊. The exam is just a starting point, and every step you take brings you closer to relief.
Kevin Galligan
October 15, 2025 AT 14:09Oh yeah, because sitting still for a few minutes is exactly what every busy person dreams of doing-kudos for actually getting it done, though!
Dileep Jha
October 16, 2025 AT 17:56While the conventional paradigm posits the pelvic exam as a preliminary heuristic, one could argue that its diagnostic yield is suboptimal without adjunctive biomarker profiling and high‑resolution imaging modalities, rendering it a merely adjunctive interrogation rather than a definitive assessment.