Missing a dose of your child’s medication can feel like a crisis. Your heart races. Did you just ruin their treatment? Should you give two doses now to make up for it? The truth is, never double a dose-and that’s just the start. Handling missed pediatric medication doses safely isn’t about guesswork. It’s about knowing the clock, the drug, and the child’s unique needs.
Timing Matters More Than You Think
Not all medications work the same way when a dose is late. The rules change based on how often your child takes it. For a once-daily medicine-like some antibiotics or seizure meds-if you realize the dose was missed within 12 hours, give it. If it’s been more than 12 hours, skip it. Don’t try to catch up. Giving two doses at once can overload a child’s system. Their liver and kidneys aren’t as strong as an adult’s, and they process drugs slower. A 2023 study from Children’s Wisconsin found that doubling doses in children under 12 increases the risk of severe reactions by 278%.
Twice-daily meds? The window shrinks to 6 hours. If you remember 5 hours after the missed dose, give it. If it’s been 7 hours, skip it and wait for the next scheduled time. Three times a day? You have only a 3-hour window. Four times a day? Just 2 hours. For meds given every 2 to 4 hours-like pain relievers or seizure rescue meds-if you miss a dose by more than 2 hours, skip it entirely. These are high-risk situations. Overdosing can lead to breathing problems, seizures, or even coma.
Some Medicines Can’t Wait
Not all missed doses are equal. Cancer treatments, immunosuppressants, and certain heart medications are different. For oncology drugs, even one missed dose can reduce treatment effectiveness. If your child is on chemotherapy or a targeted cancer therapy and misses a dose, call their oncology team immediately. Don’t wait. Don’t guess. Don’t assume it’s fine. These medications are tightly scheduled for a reason. Delaying or skipping can allow cancer cells to regrow.
Same goes for seizure medications like phenytoin or valproic acid. Missing even one dose can trigger a breakthrough seizure. If you miss one, give it as soon as you remember-but only if it’s within the safe window. After that, skip it and resume the next dose on time. Never double up. Your child’s brain is more sensitive to fluctuations in drug levels than you realize.
Why Doubling Is Dangerous
You might think, “I just want to get back on track.” But doubling a dose doesn’t help. It hurts. Children’s bodies are smaller. Their organs are still developing. A dose that’s safe once can become toxic twice. Morphine, for example, is commonly used in hospitals for pain, but in home settings, weight-based dosing errors happen in 73.8% of cases. That’s not because parents are careless-it’s because they’re using age instead of weight. A 2021 study showed that using a length-based resuscitation tape cuts weight estimation errors by 42%. That’s why accurate weight matters more than age.
And it’s not just opioids. Even common meds like ibuprofen or acetaminophen can cause liver or kidney damage if given too often. One parent on Reddit admitted to doubling doses “just to stay on schedule.” That’s not rare. In fact, 63% of caregivers in online parenting groups say they’ve done it. But the risk isn’t theoretical. Emergency rooms see children with drug toxicity every week because someone tried to make up for a missed dose.
How to Avoid Mistakes Before They Happen
Prevention beats correction. Use an oral syringe-not a teaspoon-for liquid meds. The FDA says household spoons vary so much that 22% of dosing errors come from using them. A syringe gives you precision. Label each bottle with your child’s name, the drug, and the exact dose in milliliters. Write it down. Don’t rely on memory.
For kids on multiple meds, color-coded charts work. Boston Children’s Hospital found that using red for morning, blue for afternoon, and green for night reduced missed doses by 44%. Tape the chart to the fridge. Show it to every caregiver-grandparents, babysitters, school nurses. Make sure they know what to do if a dose is missed.
Use a medication tracker app. The American Academy of Pediatrics launched a free app in 2023 called the Pediatric Medication Safety Calculator. You enter the drug, the frequency, and how late you are. It tells you: give it, skip it, or call the doctor. In beta testing, it improved caregiver decisions by 83%.
What to Do When You’re Confused
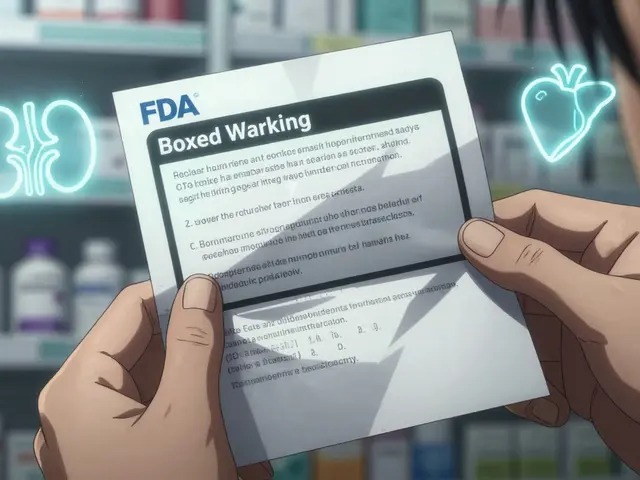
Here’s the hard truth: many drug labels don’t even say what to do if you miss a dose. A 2021 review found that 25% of high-risk pediatric medications had no missed-dose instructions in the patient leaflet. That’s not a typo. It’s a system failure. So when you’re unsure, call your pediatrician or pharmacist. Don’t Google it. Don’t ask a friend. Don’t wing it.
Ask: “Is this a high-alert medication?” “What’s the safe window for a missed dose?” “Should I call if it’s been more than X hours?” Write down their answer. Keep it with the meds. If you’re in a rush, send a text or email for confirmation. Having it in writing protects you and your child.
Special Cases: Complex Needs and Rural Challenges
Children with chronic illnesses-like cerebral palsy, epilepsy, or cystic fibrosis-often take four or more medications daily. Canadian Pediatric Society data shows they have 300% more dosing errors than other kids. That’s not because their parents are less careful. It’s because the system isn’t built for complexity. Simple tools like pill organizers won’t cut it. You need a personalized plan. Work with your care team to create a visual schedule. Include photos of the pills. Note the exact time each dose is due. Use alarms on your phone. Set multiple reminders.
And if you live in a rural area, you’re at higher risk. A 2022 report found rural families have 3.2 times more medication errors than urban ones. Why? Fewer pharmacists. Less access to specialists. Longer waits for answers. If you’re in a remote area, ask your provider for a printed emergency protocol. Keep it in your wallet. Teach your partner, your sibling, your neighbor how to follow it.
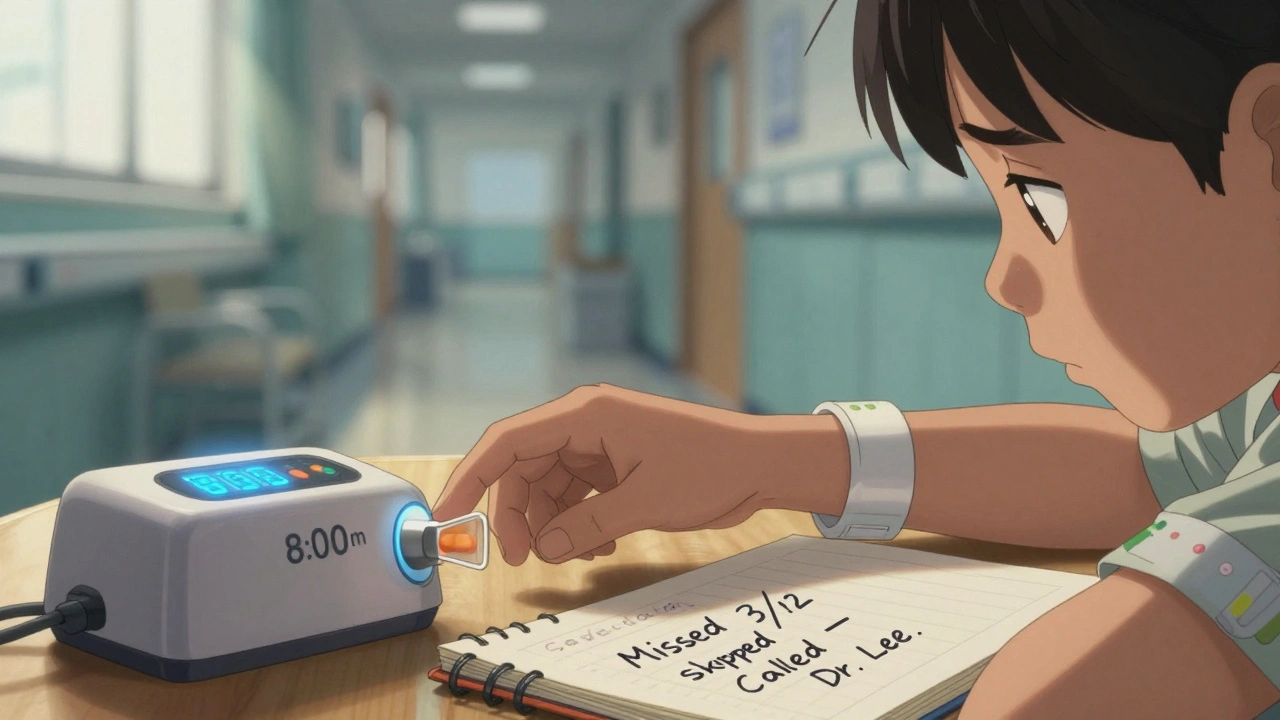
What to Do After a Missed Dose
After you’ve handled the missed dose, don’t just move on. Write it down. Note the drug, the time it was missed, the time you gave it (or didn’t), and why. Share this with your child’s doctor at the next visit. It helps them spot patterns. Maybe the schedule is too tight. Maybe the timing doesn’t fit your child’s sleep or school routine. Adjustments can be made. A once-daily dose moved from morning to bedtime might be easier to remember.
And if your child shows signs of trouble-vomiting, drowsiness, trouble breathing, unusual behavior-call 911 or go to the ER. Don’t wait. Even if you think you didn’t overdose, symptoms can appear hours later. Better safe than sorry.
Tools That Actually Help
Technology is catching up. Smart pill dispensers that lock and unlock at set times reduce missed doses by 68% in clinical trials. They’re not cheap, but some insurance plans cover them for kids with complex conditions. Ask your pharmacy. Also, look into medication reminder apps that send alerts to your phone and your partner’s. Some even sync with smartwatches.
For liquid meds, use only the syringe that came with the bottle. Never use a kitchen spoon. Even a “tablespoon” can vary by 30%. If you lose the syringe, ask for a new one. Most pharmacies give them for free.
And if your child’s school gives meds, make sure the nurse has a copy of the dosing schedule and knows exactly what to do if a dose is missed during the day. Don’t assume they know. Show them. Ask them to repeat it back.
Final Rule: When in Doubt, Skip It
The safest move 90% of the time is to skip the missed dose and wait for the next one. It’s counterintuitive. You want to fix it. But in pediatric medicine, less is often more. Your child’s body doesn’t need to be “caught up.” It needs to be stable. One missed dose won’t undo weeks of treatment. But one doubled dose could land them in the hospital.
Keep a small notebook by the medicine cabinet. Write down every missed dose, what you did, and what the doctor said. Over time, you’ll start to see patterns. You’ll know which meds are forgiving and which aren’t. You’ll stop panicking. You’ll stop guessing. And most importantly, you’ll keep your child safe.
What should I do if I miss my child’s antibiotic dose?
If it’s been less than half the time until the next dose, give it right away. For a twice-daily antibiotic, that’s within 6 hours. If it’s been longer, skip it. Never double the dose. Completing the full course is important, but giving too much at once is more dangerous than missing one dose.
Can I give a missed dose at bedtime if I forgot during the day?
Only if it’s within the safe window for that medication. For example, if your child takes a once-daily medicine at 8 a.m. and you remember at 8 p.m., that’s 12 hours-so skip it. If you remember at 6 p.m., that’s 10 hours, so give it. But never give a dose right before bed if it’s meant to be given during the day unless your doctor says it’s okay. Some meds cause drowsiness or need to be taken with food at specific times.
Is it safe to use a kitchen spoon to measure liquid medicine?
No. Kitchen spoons vary widely in size. A tablespoon can be anywhere from 14 to 21 milliliters. That’s a 50% difference. Always use the oral syringe or measuring cup that came with the medicine. If you lost it, ask your pharmacy for a new one-they’ll give it to you for free.
What if my child vomits right after taking a dose?
If your child vomits within 15 to 20 minutes of taking the medicine, it’s likely the dose didn’t absorb. Call your doctor. If it’s been more than 30 minutes, the medicine was probably absorbed, so don’t give another dose. Giving a second dose too soon can cause overdose. Always check with your provider before repeating a dose.
Do I need to call the doctor every time I miss a dose?
No-not every time. For most routine meds, following the time-based rules (skip if over the window) is enough. But call immediately if your child is on cancer meds, seizure drugs, insulin, or heart medications. Also call if you’re unsure, if your child shows side effects, or if you miss more than one dose in a row. It’s better to be safe.
Why do some medicine labels not say what to do if I miss a dose?
Many drug manufacturers don’t include missed-dose instructions on pediatric labels, even though it’s a major safety issue. A 2021 review found that 25% of high-risk pediatric medications had no guidance at all. This is changing, but slowly. Until then, always ask your doctor or pharmacist for clear instructions. Don’t rely on the bottle.
How can I prevent missed doses in the future?
Use alarms on your phone set for each dose. Create a color-coded chart and hang it where you see it every day. Use an oral syringe and measure every dose. Ask your pharmacist for a pill organizer if your child takes multiple meds. And don’t be afraid to ask for help-whether from family, school nurses, or apps like the AAP’s Pediatric Medication Safety Calculator.



Gillian Watson
December 4, 2025 AT 07:15Simple. Effective.
Martyn Stuart
December 5, 2025 AT 12:37Shofner Lehto
December 7, 2025 AT 05:03Chase Brittingham
December 7, 2025 AT 23:40Bill Wolfe
December 8, 2025 AT 04:19michael booth
December 9, 2025 AT 14:53Rudy Van den Boogaert
December 9, 2025 AT 19:44Jordan Wall
December 11, 2025 AT 08:06Yasmine Hajar
December 11, 2025 AT 20:28Ashley Elliott
December 13, 2025 AT 19:56Chad Handy
December 14, 2025 AT 20:22