When you can’t sleep, your mind doesn’t rest. It races. It replays conversations. It fears tomorrow. For millions of people with depression or anxiety, insomnia isn’t just a side effect-it’s the engine driving the whole cycle. You feel tired, irritable, hopeless. You try to sleep more, but lying there only makes it worse. You start to believe you’ll never sleep well again. And that belief? It keeps you awake.
Insomnia Isn’t Just a Symptom-It’s a Cause
For years, doctors treated insomnia as a side effect of depression or anxiety. If you were sad or anxious, you couldn’t sleep. Fix the mood, and sleep would follow. But research has turned that idea upside down. A 2025 study in Frontiers in Psychiatry found that people with chronic insomnia are 40 times more likely to develop severe depression than those who sleep well. That’s not correlation. That’s causation. Insomnia doesn’t just come with depression-it makes depression worse, longer, and harder to treat. The same is true for anxiety. When your brain is stuck in overdrive at night, it rewires itself. Stress hormones like cortisol and CRH stay elevated. Your nervous system stays on high alert. Even if your daytime worries fade, your body still thinks it’s in danger. And that keeps you awake. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) now recognizes insomnia as both a symptom and an independent disorder. That’s a big deal. It means treating sleep isn’t optional-it’s essential.CBT-I: The Gold Standard That Actually Works
There’s one treatment that stands above all others: Cognitive Behavioral Therapy for Insomnia, or CBT-I. It’s not a pill. It’s not a supplement. It’s a structured, science-backed program that changes how you think about and behave around sleep. CBT-I isn’t magic. It’s six to eight weekly sessions, each about an hour long. You work with a therapist-or use a digital platform-to tackle four core areas:- Stimulus control: Your bed is for sleep and sex only. No scrolling, no working, no lying there worrying. If you’re not asleep in 20 minutes, get up. Go sit in another room. Come back only when you’re sleepy.
- Sleep restriction: You’re probably spending too much time in bed. If you only sleep 5 hours a night, you’re not supposed to be in bed for 8. You reduce your time in bed to match your actual sleep. It’s hard at first-you’ll feel exhausted. But over time, your sleep becomes more efficient.
- Relaxation training: Deep breathing, progressive muscle relaxation, mindfulness. These aren’t fluffy wellness tricks. They lower your heart rate, calm your nervous system, and break the cycle of nighttime anxiety.
- Cognitive therapy: You learn to challenge thoughts like “I’ll never sleep again” or “If I don’t sleep tonight, my whole day will be ruined.” These beliefs keep you tense. And tension keeps you awake.
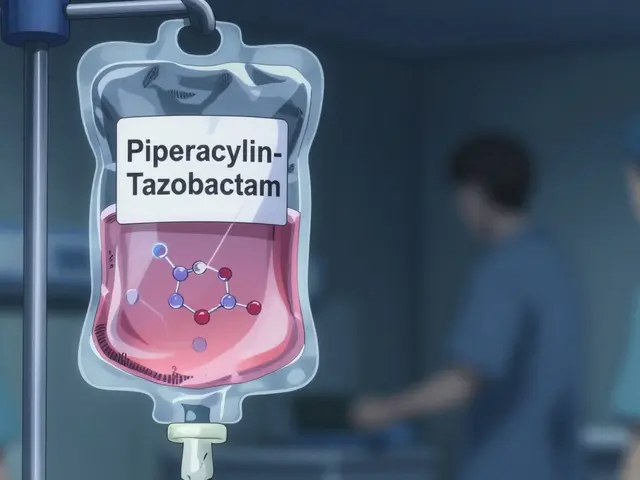
Why Pills Like Zolpidem Fall Short
You’ve probably heard of Ambien, Lunesta, or other sleep meds. They work-short term. You fall asleep faster. You might even sleep longer. But here’s the catch: they don’t fix the root problem. They mask it. A 2025 study in Nature Scientific Reports compared CBT-I to zolpidem. Both improved sleep and mood in the first few weeks. But after six months? The people who did CBT-I stayed better. The people who took pills? Their insomnia and anxiety came back. And often worse. Why? Because pills don’t change your thoughts. They don’t retrain your brain. They just sedate you. And your brain learns to rely on them. You can’t just quit cold turkey. Withdrawal can make sleep even harder. CBT-I teaches you to sleep without drugs. And once you learn it, you don’t need to keep doing it forever. The skills stick.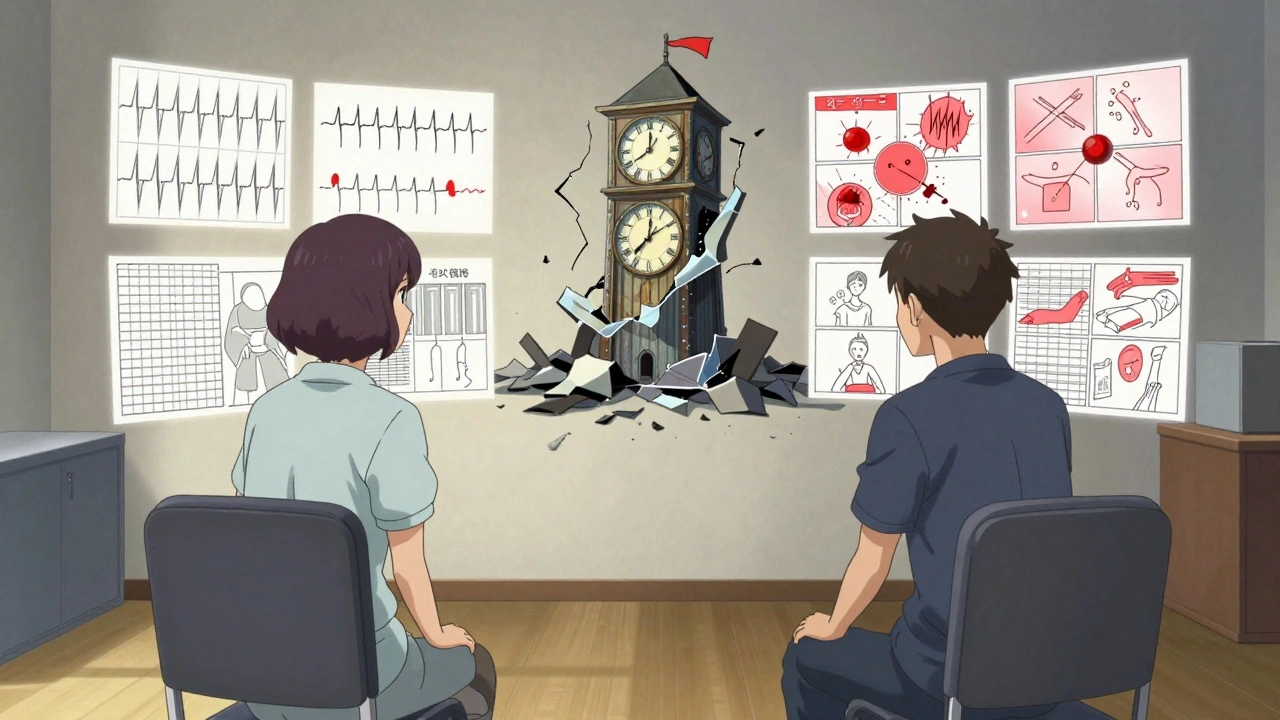
Digital CBT-I: Therapy You Can Access From Your Couch
Finding a CBT-I therapist can be hard. In the U.S., fewer than 5% of psychologists are trained in it. Insurance often doesn’t cover it. Waitlists are months long. That’s where digital platforms like Sleepio and SHUTi come in. These are online programs built by sleep scientists. They walk you through CBT-I step by step, with videos, interactive tools, and daily check-ins. One study showed that people using Sleepio had a 57% lower chance of developing moderate-to-severe depression compared to those who just read sleep tips. Another found that 76% of users saw a clinically meaningful drop in insomnia severity. These platforms aren’t perfect. You still need to do the work. You still have to track your sleep. But they’re far better than nothing. And they’re growing fast. Telehealth CBT-I use jumped 300% between 2019 and 2022.What Happens When You Don’t Treat Insomnia
Ignoring sleep doesn’t make depression or anxiety go away. It makes them worse. During the pandemic, Columbia University found that one in three adults had clinical insomnia symptoms. That’s more than double pre-pandemic rates. And those with insomnia were far more likely to report high levels of psychological distress. Without treatment, insomnia becomes a trap:- You feel too tired to exercise, so you get less endorphins.
- You skip meals or eat junk because you’re too drained to cook.
- You cancel plans because you’re exhausted.
- You feel guilty for not sleeping, which makes you more anxious.
- The cycle tightens.

Barriers to Getting Help
You might be thinking: “This sounds great, but how do I get it?” The truth? Access is still a huge problem. - Only 1-2% of people with insomnia get CBT-I. - Insurance often won’t cover it unless you have a specific diagnosis. - Many therapists don’t offer it. - Digital platforms cost money, and not everyone can afford them. Kaiser Permanente started screening all depression patients for insomnia in 2022. They linked sleep problems directly to care. Result? A 22% drop in depression relapses. That’s what’s possible when systems change. But until then, you have to be your own advocate.What You Can Do Right Now
You don’t need to wait for a therapist to start helping your sleep. Try these steps today:- Write down your sleep schedule. What time do you get in bed? What time do you actually fall asleep? What time do you wake up? Do this for a week.
- Get out of bed if you’re not asleep after 20 minutes. Go to another room. Read a book under dim light. Don’t check your phone.
- Don’t nap after 3 p.m. Even a 20-minute nap can wreck your nighttime sleep if you have insomnia.
- Limit caffeine after noon. It stays in your system for 6-8 hours.
- Try a 5-minute breathing exercise before bed. Breathe in for 4 counts, hold for 4, breathe out for 6. Repeat. This calms your nervous system.
The Bigger Picture
Sleep isn’t just rest. It’s repair. It’s emotional regulation. It’s memory consolidation. It’s your brain cleaning out the toxins of the day. When you treat insomnia in someone with depression or anxiety, you’re not just helping them sleep. You’re giving their brain a chance to heal. And the data is clear: fixing sleep doesn’t just improve mood-it prevents relapse. It saves money. It saves lives. This isn’t about sleeping more hours. It’s about sleeping better. And that’s something anyone can learn.Can insomnia cause depression, or is it just a symptom?
Insomnia isn’t just a symptom of depression-it can cause it. Research shows people with chronic insomnia are 40 times more likely to develop severe depression. Treating insomnia reduces the risk of new depressive episodes, proving it’s a causal factor, not just a side effect.
Is CBT-I better than sleeping pills for depression and anxiety?
Yes. While sleeping pills like zolpidem help you fall asleep faster, they don’t fix the underlying thoughts and behaviors keeping you awake. CBT-I teaches skills that last. Studies show people who complete CBT-I have much lower relapse rates and better long-term mood outcomes than those who rely on medication alone.
How long does CBT-I take to work?
Most people start seeing improvements in 2-4 weeks. Full results usually take 6-8 weeks. The hardest part is the first week-sleep restriction can make you feel exhausted. But after that, sleep becomes deeper and more consistent. The key is sticking with it.
Can I do CBT-I on my own with an app?
Yes. Digital CBT-I programs like Sleepio and SHUTi are clinically proven to work. They follow the same evidence-based steps as in-person therapy. While working with a therapist offers more support, apps are a powerful, accessible option-especially if you can’t find a specialist nearby.
Will treating insomnia help my anxiety too?
Absolutely. Anxiety and insomnia feed each other. When you break the cycle of nighttime worry with CBT-I, your daytime anxiety often improves too. Studies show CBT-I reduces anxiety symptoms as much as it improves sleep, because your nervous system finally gets a chance to reset.
What if CBT-I doesn’t work for me?
About 30-40% of people don’t fully recover with CBT-I alone. That doesn’t mean it failed-it means you might need a combination approach. Adding a short-term antidepressant or working with a specialist to adjust your plan can help. The goal isn’t perfection-it’s progress. Even small improvements in sleep can make a big difference in how you feel during the day.
Is CBT-I covered by insurance?
Some plans cover it, especially if you have a diagnosis of insomnia disorder. Many don’t. Digital platforms often cost $50-$150 per month, but some employers or clinics offer them for free. Ask your provider or check if your workplace has a wellness program that includes sleep therapy.
How do I know if I have insomnia disorder?
You may have insomnia disorder if you’ve had trouble falling or staying asleep at least three nights a week for three months or more, and it’s causing daytime problems like fatigue, mood swings, or trouble focusing-even when you have the chance to sleep. If this sounds familiar, talk to your doctor or a sleep specialist.



Ada Maklagina
December 6, 2025 AT 00:56Been doing the 20-minute rule for a week now. Got up last night, read a chapter of Dune under a lamp, came back, fell asleep in 8 minutes. No pills. No magic. Just discipline.
Feels weird to say it but I actually miss the old me-the one who didn’t hate bedtime.
Philip Kristy Wijaya
December 6, 2025 AT 15:26Insomnia is not a disorder it is a lifestyle choice made by people who refuse to accept that modern life is chaotic and sleep is a bourgeois luxury
My grandfather slept four hours a night and built three companies
You want to fix sleep stop watching TikTok at 2am and stop treating your bed like a Netflix lounge
Manish Shankar
December 8, 2025 AT 02:20As someone who has lived with chronic insomnia for over a decade, I can confirm that CBT-I is the only intervention that brought lasting relief. The sleep restriction phase was brutal-my productivity collapsed for two weeks-but by week five, I was sleeping six hours without effort. The cognitive reframing changed how I view rest. It is not a reward for productivity; it is the foundation of it.
Harry Nguyen
December 8, 2025 AT 08:49Of course CBT-I works-because it requires effort and discipline
Unlike the woke therapy culture that wants you to believe you deserve a pill to fix your poor life choices
Wake up. Your brain isn’t broken. You’re just lazy and addicted to dopamine
Katie Allan
December 9, 2025 AT 21:01This is the most important public health conversation we’ve had in a decade.
Not because it’s new-but because we’ve ignored it for so long.
When we treat sleep like an afterthought, we’re telling people their mental health doesn’t matter.
CBT-I isn’t therapy-it’s a civil right.
And if your insurance won’t cover it, you’re not broken-you’re in a broken system.
James Moore
December 11, 2025 AT 16:51Let’s be clear: the pharmaceutical-industrial complex has spent billions convincing people that sleep is a chemical imbalance, when in fact it is a behavioral, cognitive, environmental, and spiritual crisis-and yet we still reach for Ambien because it’s easier than facing the fact that we live in a society that glorifies burnout and pathologizes rest
And now we’re told that sleep is a disorder? No-it’s a symptom of a civilization that has forgotten how to be human.
Kylee Gregory
December 13, 2025 AT 11:33I tried CBT-I after years of failed meds. The sleep restriction part made me feel like a zombie. But I stuck with it. Now I sleep 7 hours most nights. I still have bad nights. But now I don’t panic. I just sit. Breathe. Wait. And it always comes back. That’s the real gift-not perfect sleep, but peace with imperfect sleep.
Laura Saye
December 13, 2025 AT 11:33The neurobiological feedback loop between hyperarousal and rumination is well-documented in the literature on sleep-wake regulation and HPA axis dysregulation. CBT-I modulates cortical-thalamic connectivity and reduces nocturnal cortisol secretion, thereby restoring homeostatic sleep pressure. Digital platforms enhance adherence through behavioral reinforcement algorithms, which align with operant conditioning principles. The longitudinal data from the Sleepio RCTs demonstrate significant reductions in PHQ-9 scores, suggesting a neuroplastic reorganization of affective processing networks during sleep consolidation.
Carole Nkosi
December 15, 2025 AT 03:38Oh so now we’re blaming people for not sleeping because they’re too anxious? What about the people who work three jobs? Who live in noisy apartments? Who don’t have a bed? Who don’t have access to therapy? You talk about CBT-I like it’s a cure-all, but for most of us, it’s a fantasy. Sleep is a privilege. And you’re just another person with a couch and a therapist telling us to fix ourselves while the system burns.
Stephanie Bodde
December 15, 2025 AT 20:24YOU GOT THIS 💪
First week of CBT-I is the hardest-I cried every night. But you’re not failing. You’re rewiring. Every time you get up after 20 mins? That’s courage. Every time you put your phone away? That’s power. You’re not broken. You’re becoming. Keep going. I’m rooting for you.
luke newton
December 16, 2025 AT 09:02Why do you think so many people can’t sleep? Because they’re too busy feeling sorry for themselves
My dad worked 16-hour shifts in a steel mill and slept 5 hours a night
He didn’t have a therapist
He didn’t have an app
He just got up and did what needed to be done
Stop treating your mind like a fragile flower
William Chin
December 17, 2025 AT 21:33It is imperative to recognize that the medicalization of sleep disturbance represents a profound epistemological shift in psychiatric nosology. The DSM-5’s reclassification of insomnia as a discrete disorder is not merely diagnostic-it is ontological. It reconfigures the subject as a locus of behavioral regulation rather than a passive recipient of psychopathological contagion. Consequently, CBT-I functions not as therapy, but as a disciplinary technology of the self, aligning the individual with normative circadian rhythms prescribed by institutional authority.
Chris Brown
December 18, 2025 AT 21:56CBT-I? That’s just the woke version of ‘just sleep’
They took a simple thing-sleep-and turned it into a 6-week program with worksheets and breathing exercises because they don’t trust people to be responsible for their own lives
Meanwhile, people are getting real help from magnesium, melatonin, and cutting out screens
But no-let’s make it complicated so we can sell more therapy
Krishan Patel
December 20, 2025 AT 04:06Insomnia is not caused by stress. It is caused by moral weakness. You do not sleep because you lack discipline. You do not sleep because you prioritize entertainment over rest. You do not sleep because you are weak. And now you want a pill? A program? A therapist? No. You need a boot to the backside and a 5 a.m. alarm. Sleep is earned. Not granted. Stop begging for help and start being a man.
sean whitfield
December 20, 2025 AT 13:35They say CBT-I works
But have you ever wondered who profits from this?
Therapists get paid
App companies get subscriptions
Doctors get referrals
Meanwhile you’re still awake at 3am
And they’re selling you the next version of the same lie
Wake up. Sleep is a myth. Your brain is just wired wrong. And no app will fix that.