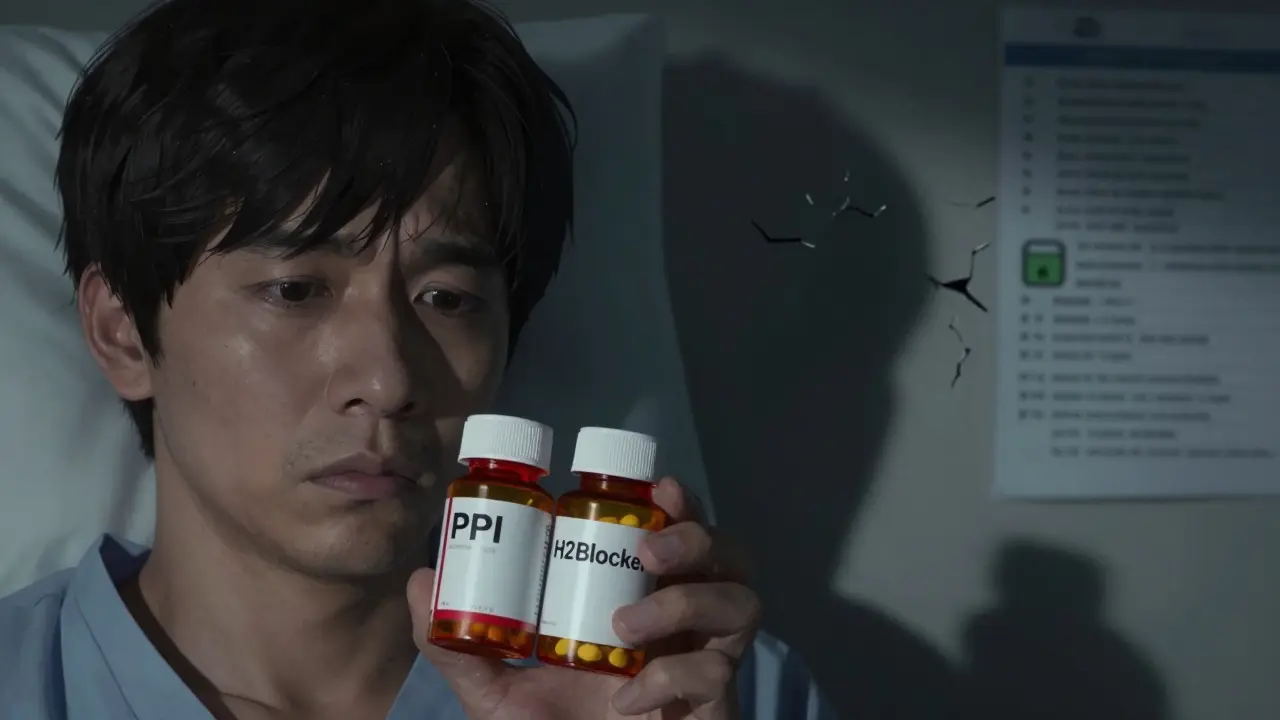
Many people take acid-reducing meds without knowing they might be taking two that cancel each other out - or even make things worse. If you’re on both an H2 blocker and a proton pump inhibitor (PPI), you’re not alone. About 1.2 million hospitalized patients in the U.S. get both every year. But here’s the problem: for most people, this combo doesn’t help - and it could be hurting you.
How H2 Blockers and PPIs Actually Work
H2 blockers like famotidine (Pepcid) and cimetidine (Tagamet) work by blocking histamine, a chemical that tells your stomach to make acid. They start working in about an hour and last 6 to 12 hours. They’re good for quick relief, like after a spicy meal.
PPIs - such as omeprazole (Prilosec), esomeprazole (Nexium), and pantoprazole (Protonix) - work differently. They shut down the actual acid-making pumps in your stomach cells. This is a deeper, longer-lasting stop. But they don’t work right away. It takes 2 to 5 days to reach full power. Once they do, they suppress acid by 90-98% - far more than H2 blockers ever can.
Here’s the twist: PPIs suppress acid so much that histamine doesn’t even have a chance to trigger acid production. And that’s the problem. H2 blockers need histamine to be active in order to work. If the PPI has already silenced the signal, the H2 blocker is basically standing by with no job to do.
The Evidence Says: No Real Benefit for Most People
A 2022 review of 12 clinical trials with nearly 3,000 patients found no meaningful improvement in symptoms when H2 blockers were added to PPIs for GERD. The American College of Gastroenterology’s 2022 guidelines say outright: “Long-term combination therapy does not offer additional benefit.”
One study measured acid levels in the stomach of patients on omeprazole plus ranitidine. The extra H2 blocker only lowered acid exposure by 5% - and only during nighttime. That’s not enough to justify the risk. For most people, doubling up doesn’t mean better relief. It just means more pills, more cost, and more side effects.
Side Effects You Might Not Know About
PPIs are linked to real, serious risks - especially with long-term use. A 2014 study of nearly 80,000 ICU patients found PPI users had a 30% higher risk of hospital-acquired pneumonia and a 32% higher risk of Clostridium difficile infection. That’s not a small risk. It’s life-threatening.
Even more surprising? PPIs were linked to a 22% higher risk of gastrointestinal bleeding compared to H2 blockers - the exact opposite of what you’d expect if PPIs were “stronger” protectors.
For people with kidney disease, the danger is even clearer. A 2021 study of over 3,600 patients found those on PPIs had a 28% higher chance of progressing to end-stage kidney disease than those on H2 blockers. That’s not a coincidence. The body doesn’t handle long-term acid suppression well.
And then there’s the side effect list: headaches (23% of users), diarrhea (18%), and nutrient deficiencies like low magnesium, B12, and calcium. Many people don’t realize their joint pain, brittle nails, or fatigue could be tied to their daily pill.
Why Do Doctors Still Prescribe This Combo?
It’s not because the science supports it. It’s because of habit, fear, and marketing.
Doctors sometimes add an H2 blocker at night because they’re worried about “nocturnal acid breakthrough” - when acid surges after midnight. But here’s the catch: only about 10-15% of patients on PPIs actually have this problem. And even then, you need to confirm it with a 24-hour pH monitor. Most people never get tested.
Meanwhile, the U.S. spends $1.5 billion a year on this unnecessary combo. PPIs make up 78% of all acid-suppressing prescriptions - even though H2 blockers are cheaper, safer, and just as effective for many conditions like mild heartburn or stress ulcer prevention.
Who Might Actually Benefit?
There’s one real exception: patients with documented nocturnal acid breakthrough. That means they’ve had symptoms like nighttime heartburn, and a pH test showed their stomach stayed too acidic (below pH 4) for more than an hour between midnight and 6 a.m. - despite taking a full dose of PPI twice daily.
Even then, the H2 blocker should be a short-term fix. The American College of Gastroenterology recommends trying it for only 4 to 8 weeks. If symptoms don’t improve, stop it. Don’t keep it forever.
The VA’s guidelines say it plainly: if you’re on both, you need documentation. No notes? No justification. Time to reassess.
What You Should Do
If you’re taking both an H2 blocker and a PPI:
- Ask your doctor: “Why am I on both?” If they say “just because,” push back.
- Ask if you’ve ever had a pH test to confirm nighttime acid breakthrough.
- Check if you’re on the lowest effective dose of PPI. Many people stay on high doses for years without needing them.
- Ask about a “PPI time-out” - stopping the drug for 2-4 weeks to see if you still need it.
- If you’ve been on this combo for more than 3 months, ask if you can try stopping the H2 blocker first.
Most people can safely taper off one of the two. You might feel some rebound heartburn for a few days - that’s normal. It doesn’t mean you’re addicted. It means your stomach is readjusting.
The Bigger Picture
Medications aren’t always better when stacked. Sometimes, less is more. H2 blockers have been around since the 1970s. They’re inexpensive, well-studied, and safer for long-term use than PPIs. Yet, because PPIs were marketed as “stronger,” they became the default - even when they weren’t needed.
Now, regulators are catching on. CMS (Centers for Medicare & Medicaid Services) will start penalizing hospitals in 2024 if more than 15% of their patients are on inappropriate dual acid suppression. That’s a big shift.
And research is finally asking the right questions. A 2023 NIH study is looking at genetic markers to see who might truly benefit from the combo. But for now, the answer is simple: if you don’t have proof you need both, you probably don’t.
Don’t assume more medication = better care. Sometimes, it’s just more risk - and a bigger bill.



Josh Kenna
January 17, 2026 AT 17:47I’ve been on omeprazole for 5 years and added famotidine at night because my doc said ‘just in case’-turns out I never got a pH test. This post blew my mind. Stopped the H2 blocker last week. Rebound heartburn for 3 days? Yeah. But now I feel way less bloated and my joints don’t ache anymore. Who knew?
Lewis Yeaple
January 19, 2026 AT 02:32It is imperative to note that the concomitant administration of histamine H2-receptor antagonists and proton pump inhibitors is not only pharmacodynamically redundant, but also potentially deleterious due to the suppression of gastric acid-mediated defense mechanisms. The clinical evidence, as cited in the 2022 ACG guidelines, is unequivocal: no additive benefit exists in the majority of patients. Furthermore, the increased risk of C. diff and pneumonia is not speculative-it is statistically significant and reproducible across multiple cohort studies.
Jake Rudin
January 20, 2026 AT 01:48Think about it: we’ve turned our stomachs into sterile labs… and then wonder why our immune system forgets how to fight anything. Acid isn’t the enemy-it’s the gatekeeper. When you shut it down for years, you’re not ‘healing’-you’re starving your microbiome, your nutrient absorption, your natural defenses. And then we blame the body for ‘failing’… when it was never given a chance to function. We’re not treating disease-we’re treating symptoms with a sledgehammer and calling it medicine.
Phil Hillson
January 21, 2026 AT 10:47THIS IS WHY AMERICA IS BROKE. Doctors prescribe this junk because they’re lazy and Big Pharma pays them to. I got prescribed both after a 10-minute visit. No tests. No questions. Just ‘take these.’ Now I’m on 5 meds for side effects from the 2 meds I was on for heartburn. This is a scam. Someone needs to sue someone.
Erwin Kodiat
January 21, 2026 AT 20:50Really appreciate this breakdown. I used to think more pills = more healing. Turns out, my body just needed to breathe. Went off the combo cold turkey after reading this-rebound was rough but worth it. My skin cleared up, my energy came back. Sometimes the body just needs space to fix itself. Less is more, always.
Valerie DeLoach
January 23, 2026 AT 20:17As someone who’s spent years managing GERD without medication, I want to emphasize: lifestyle changes-elevating the head of your bed, avoiding late meals, reducing alcohol and caffeine-are often more effective and safer than any drug combo. Many patients are never even offered these options. The medical system prioritizes prescriptions over education. This needs to change.
Christi Steinbeck
January 24, 2026 AT 03:19STOP TAKING BOTH. I was on them for 7 years. Started tapering after this post. Felt like a new person. No more brain fog. No more brittle nails. My doctor said I was ‘addicted’-nope. I was just misinformed. If you’re on this combo, you owe it to yourself to ask for a time-out. You’re not weak for wanting to feel better-you’re smart.
Jacob Hill
January 25, 2026 AT 12:00Interesting. I’m curious-how many of these patients were also on NSAIDs? Because I’ve seen cases where the combo was actually justified for ulcer prophylaxis in high-risk patients… but only if they’re on daily aspirin or ibuprofen. Maybe the problem isn’t the combo-it’s that we’re not screening for the right risk factors before prescribing?
Jackson Doughart
January 26, 2026 AT 02:50Thank you for this. I’ve been quietly questioning my own regimen for months. My doctor dismissed my concerns as ‘overthinking.’ But after reading this, I scheduled a follow-up. We’re doing a 4-week PPI pause next month. I’m nervous-but hopeful. It’s not about rejecting medicine. It’s about respecting the body’s intelligence.
Tracy Howard
January 26, 2026 AT 09:37Of course Americans are overdosing on PPIs-you’re a nation of sugar addicts who think a pill fixes everything. In Canada we don’t even prescribe this combo unless there’s a documented GI bleed history. You people treat your stomach like a broken faucet and keep turning the knob harder until it explodes. Wake up.