ACE Inhibitor Safety Checker
Assess ACE Inhibitor Safety
This tool helps determine if ACE inhibitors are safe to use based on your kidney status and risk factors.
Starting an ACE inhibitor can be a simple decision for high blood pressure - until it isn’t. For some people, this common blood pressure medication can cause sudden, serious kidney damage. The reason? Renal artery stenosis. It’s not a rare edge case. It’s a well-documented, life-threatening interaction that still catches doctors off guard today.
What Happens When You Take ACE Inhibitors With Narrowed Kidney Arteries
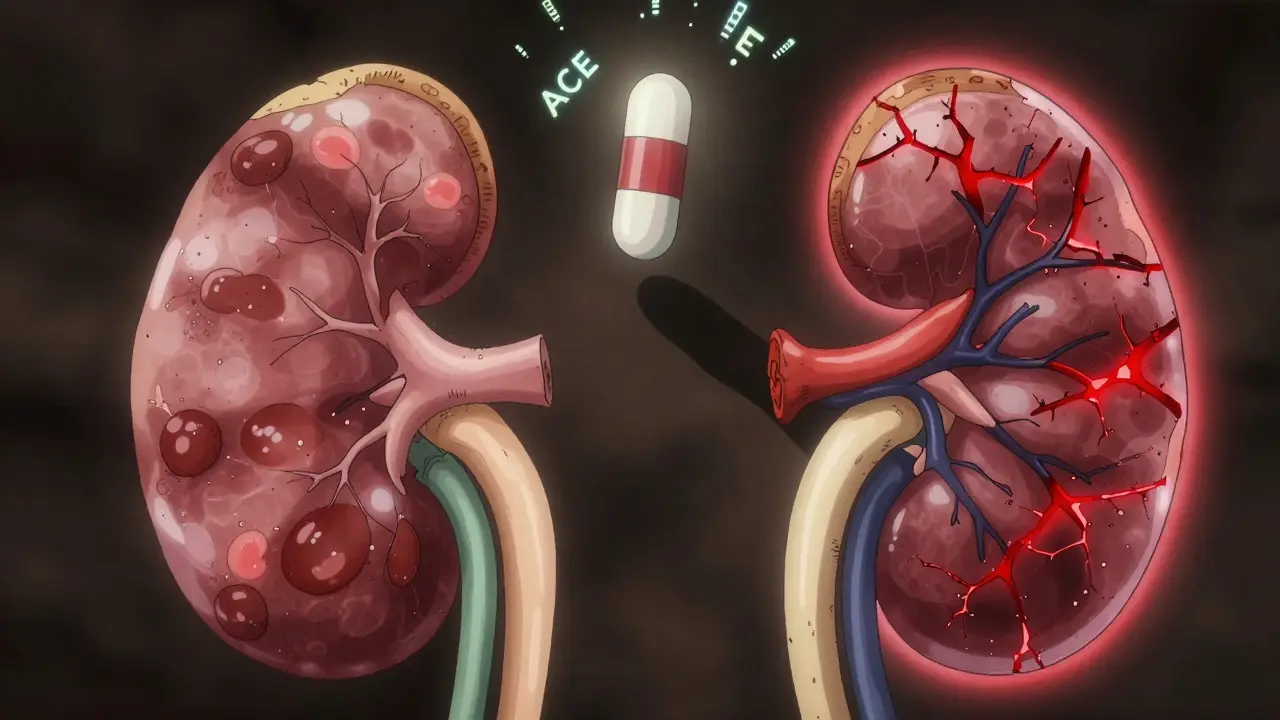
ACE inhibitors work by blocking a chemical called angiotensin II, which normally tightens blood vessels and raises blood pressure. That’s good for most people. But in someone with renal artery stenosis - where one or both kidney arteries are narrowed - angiotensin II plays a different, critical role.
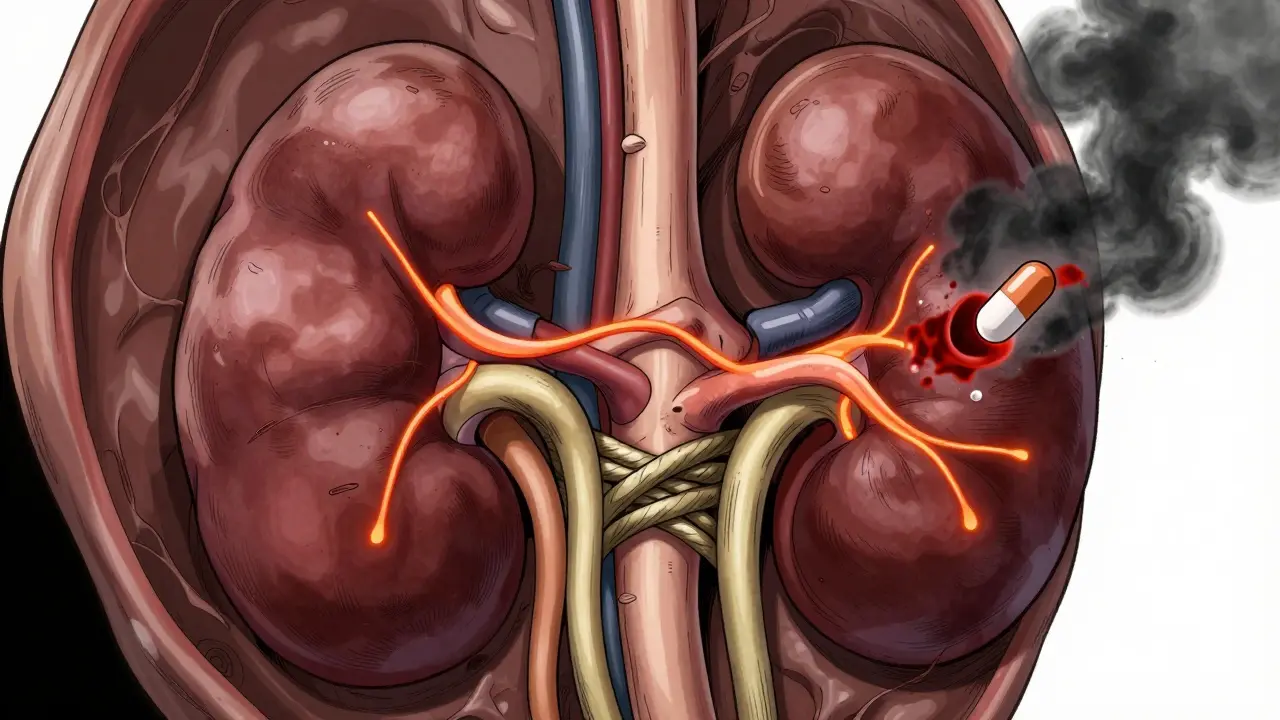
When blood flow to the kidney drops because of a blockage, the kidney thinks it’s being starved. It responds by releasing renin, which triggers angiotensin II production. That angiotensin II doesn’t just raise blood pressure overall. It specifically constricts the tiny outlet vessel (efferent arteriole) inside the kidney. This keeps pressure high inside the filtering units (glomeruli), so the kidney can still remove waste - even with less blood coming in.
Take away angiotensin II with an ACE inhibitor, and that protective constriction disappears. The efferent arteriole opens up. Glomerular pressure drops by 25-30%. Filtration slows. Creatinine rises. Kidney function crashes.
This isn’t a slow decline. It happens fast. In studies, serum creatinine jumps more than 30% within 7-10 days of starting the drug. For someone with bilateral renal artery stenosis - meaning both kidneys are affected - this can mean needing dialysis within days.
Bilateral vs. Unilateral: Why It Matters
Not all renal artery stenosis is the same. The danger is real only when both kidneys are affected, or when there’s only one working kidney.
If you have stenosis in one kidney but the other kidney is healthy and normal, your body can compensate. The good kidney picks up the slack. ACE inhibitors can often be used safely here - with close monitoring. That’s why doctors don’t automatically rule out these drugs for everyone with a narrowed artery.
But if both arteries are blocked, or if you have a single functioning kidney (due to prior surgery, transplant, or congenital absence), the system has no backup. Block angiotensin II, and filtration collapses. That’s why the FDA and major medical societies list bilateral stenosis or stenosis in a solitary kidney as a hard contraindication for all ACE inhibitors - from captopril to lisinopril to ramipril.
What the Evidence Shows
This isn’t theoretical. It’s been proven over and over.
In a landmark 1984 study published in the New England Journal of Medicine, 12 out of 15 patients with bilateral renal artery stenosis developed acute kidney failure after taking captopril. Since then, dozens of studies have confirmed it. A 2001 micropuncture study showed angiotensin II increases resistance in the efferent arteriole by nearly 38% in stenotic kidneys - a crucial lifeline that ACE inhibitors cut.
The ASTRAL trial follow-up in 2017 gave us clear numbers: In patients with bilateral stenosis, those on ACE inhibitors saw their kidney function (eGFR) drop by an average of 18.7 mL/min/1.73m². Those not on the drugs dropped only 3.2. That’s a six-fold difference.
And it’s not just ACE inhibitors. Angiotensin receptor blockers (ARBs) like losartan and valsartan do the same thing. They block the same final pathway. If ACE inhibitors are dangerous here, so are ARBs. Many patients assume switching to an ARB is safer - it’s not.
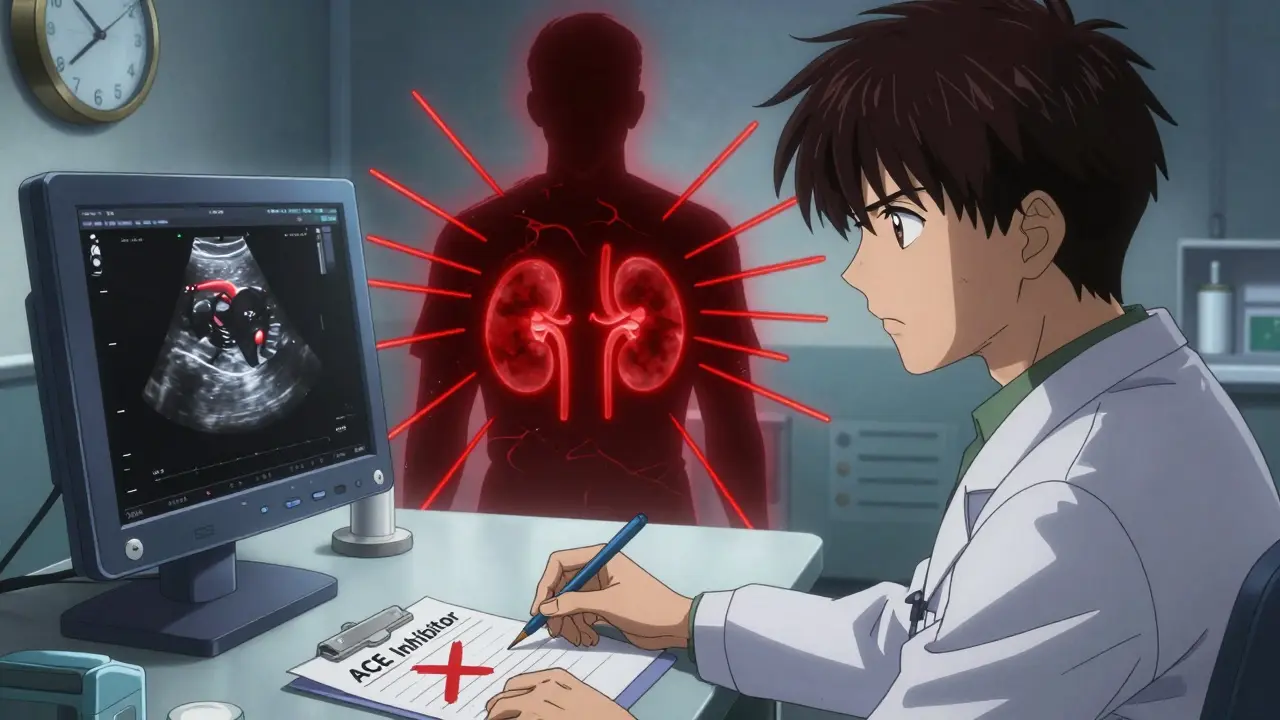
Who’s at Risk? Screening Matters
Most people with renal artery stenosis don’t know it. It often shows up after the damage is done.
High-risk groups include:
- People over 60 with new-onset or worsening high blood pressure
- Those with sudden kidney function decline after starting blood pressure meds
- Patients with abdominal bruits (a whooshing sound heard with a stethoscope over the belly)
- Anyone with unexplained kidney failure and no history of diabetes or chronic disease
Guidelines from the American Heart Association and European Society of Cardiology say you should check for stenosis before starting ACE inhibitors in these patients. The go-to test? Renal artery duplex ultrasound. It’s noninvasive, widely available, and detects significant narrowing with 86% sensitivity and 92% specificity.
Yet, a 2020 study across 15 U.S. healthcare systems found that over 22% of patients with known bilateral renal artery stenosis were still being prescribed ACE inhibitors. That’s not just a mistake - it’s a pattern.
Monitoring Isn’t Optional - It’s Life-Saving
Even if you’re not in a high-risk group, guidelines are clear: Check kidney function before starting an ACE inhibitor. Then check again in 7-10 days.
NICE guidelines (UK) and the American Heart Association both recommend testing serum creatinine and potassium levels:
- Before starting
- Within 7-10 days after starting
- After any dose increase
A rise in creatinine of more than 30% from baseline is a red flag. It doesn’t mean you have stenosis - but it means you need to stop the drug and get evaluated. In most cases, kidney function returns to normal within days of stopping the ACE inhibitor. But if the low blood flow lasts more than 72 hours, permanent damage can occur.
And if your creatinine is already above 150 micromol/L before starting? Don’t begin an ACE inhibitor without a nephrologist’s input.
What If You’re Already on an ACE Inhibitor?
If you’ve been on an ACE inhibitor for months or years and your doctor just found out you have renal artery stenosis, don’t panic. But don’t ignore it either.
If you have bilateral stenosis or a single kidney, stop the drug immediately and contact your doctor. You’ll need an alternative blood pressure strategy - maybe calcium channel blockers, diuretics, or beta-blockers. These don’t rely on the renin-angiotensin system the same way.
If you have unilateral stenosis with a healthy opposite kidney, your doctor may keep you on the ACE inhibitor - but only with close follow-up. Monthly kidney tests, strict blood pressure control, and avoiding dehydration are non-negotiable.
Why This Still Happens in 2026
It’s 2026. We have electronic health records, clinical decision support tools, and AI alerts. So why are people still getting ACE inhibitors when they shouldn’t?
Because the warning isn’t loud enough. Many doctors think renal artery stenosis is rare. It’s not. One study found 6.8% of hypertensive patients with kidney problems had significant stenosis. That’s nearly 1 in 15.
Another reason? Patients don’t know to ask. If you’re over 60, have high blood pressure that’s hard to control, or noticed your kidneys acting up after a med change - speak up. Ask: "Could I have renal artery stenosis? Should we check before starting this drug?"
This isn’t about avoiding treatment. It’s about choosing the right treatment safely. ACE inhibitors save lives - but only when used correctly.
Can ACE inhibitors cause kidney failure?
Yes - but only in specific cases. In people with bilateral renal artery stenosis or a single functioning kidney, ACE inhibitors can cause sudden, severe kidney failure by dropping the pressure needed for filtration. This is not common in healthy kidneys, but it’s a well-documented risk in these high-risk groups.
Is it safe to take ACE inhibitors if I have one narrowed kidney?
It can be - if your other kidney is healthy and working normally. Your doctor may still prescribe an ACE inhibitor in this case, but only with close monitoring of kidney function every 7-10 days after starting. If your creatinine rises more than 30%, the drug must be stopped.
Do ARBs have the same risk as ACE inhibitors for renal artery stenosis?
Yes. ARBs like losartan and valsartan block the same final pathway as ACE inhibitors. They carry the same contraindication for bilateral renal artery stenosis or stenosis in a solitary kidney. Switching from an ACE inhibitor to an ARB won’t fix the problem - it just changes the drug name.
How soon after starting an ACE inhibitor should kidney function be checked?
Guidelines from NICE and the American Heart Association recommend checking serum creatinine and potassium levels before starting the drug, then again 7-10 days after starting. A rise of more than 30% from baseline signals possible renal artery stenosis and requires immediate evaluation.
Can kidney damage from ACE inhibitors be reversed?
In most cases, yes. If caught early, stopping the ACE inhibitor allows kidney function to return to normal within days. But if low blood flow to the kidney lasts more than 72 hours, permanent damage can occur. That’s why timing matters - don’t wait for symptoms.
Who should be screened for renal artery stenosis before taking ACE inhibitors?
People over 60 with new or worsening high blood pressure, those with unexplained kidney function decline, patients with an abdominal bruit (a whooshing sound heard with a stethoscope), or anyone with sudden kidney failure without a clear cause. Screening with renal artery duplex ultrasound is recommended before starting ACE inhibitors in these groups.




Amy Le
January 7, 2026 AT 04:25So let me get this straight-we’re still letting doctors prescribe ACE inhibitors without checking for renal artery stenosis in 2026? 🤦♀️ We have AI that can predict stock markets but can’t flag a contraindication? This isn’t negligence-it’s malpractice with a side of laziness. I’ve seen this happen to my aunt. She went from 70 to dialysis in 10 days. No one asked if she had a bruit. No one checked. Now she’s on a waiting list. Thank you, healthcare system.
Pavan Vora
January 8, 2026 AT 18:14Wow, this is so important... I mean, really, really important. In India, we have so many elderly patients with hypertension, and doctors just prescribe lisinopril like candy... I have seen so many cases where creatinine rises after 5 days, and no one connects the dots... It’s like we forget basic physiology... Please, please, please check ultrasound before prescribing... 🙏
Stuart Shield
January 10, 2026 AT 01:56This is one of those quiet tragedies in medicine-no fanfare, no viral TikTok, just a slow, silent collapse of kidney function because someone didn’t pause long enough to ask, ‘What’s the story behind this BP?’ ACE inhibitors are like a Swiss Army knife-brilliant for most, catastrophic if you use the wrong blade. That efferent arteriole? It’s not a detail. It’s the last lifeline. And we’re cutting it like it’s a loose thread.
Tom Swinton
January 11, 2026 AT 07:56Listen-I’ve been in this game for 22 years, and I’ve seen too many patients crash because someone thought ‘it’s just a BP med’-NO. IT’S NOT. ACE inhibitors are not aspirin. They’re a precision tool, and if you don’t know the anatomy, you’re not a doctor-you’re a hazard. I tell my residents: if you’re about to prescribe an ACE inhibitor to someone over 60 with uncontrolled HTN, STOP. Do an ultrasound. Check the history. Ask about abdominal sounds. If you skip this, you’re not being efficient-you’re being dangerous. And if you think ARBs are safer? That’s not wisdom-that’s delusion. They’re the same damn mechanism, just dressed up in a different lab coat. I’ve had patients come back with creatinine at 4.8 because their PCP ‘switched to losartan for better tolerance.’ Tolerance? What about kidney function? What about the fact that their efferent arteriole just gave up? This isn’t a ‘maybe.’ This is a ‘never again.’
Gabrielle Panchev
January 12, 2026 AT 18:44Actually, I think this whole contraindication is overblown... I mean, if the kidney is already failing, why are we even trying to preserve it? Maybe the body knows what it’s doing... Also, aren’t we just prolonging the inevitable? And why are we so obsessed with creatinine? It’s just a number... I’ve seen people with ‘high’ creatinine live longer than those with ‘normal’ labs... Maybe we should stop medicating everything... Also, I heard the FDA is in bed with Big Pharma...
Melanie Clark
January 12, 2026 AT 20:26My neighbor’s husband died after taking lisinopril. They never tested him. They never asked. The hospital said it was ‘unavoidable.’ But I know better. I’ve read about the ASTRAL trial. I know the numbers. This is not an accident. This is a cover-up. They don’t want you to know that the same drugs that lower your BP are quietly killing your kidneys. They’re pushing these meds because they’re cheap. Because they’re profitable. Because they don’t care about you. You think your doctor is helping? They’re just following the script. The ultrasound? Too expensive. The follow-up? Too time-consuming. The truth? They’d rather kill you slowly than admit they don’t know enough. I’ve seen it. I’ve documented it. I’ve warned them. They laughed. Now he’s gone.
Venkataramanan Viswanathan
January 14, 2026 AT 20:09In India, many patients are prescribed ACE inhibitors without any baseline creatinine check. Even in teaching hospitals, the protocol is often skipped due to time constraints. This article is a wake-up call. The renal artery duplex is simple, non-invasive, and cost-effective. Why is it not mandatory? We need mandatory pre-prescription screening for patients over 55 with new-onset hypertension. This is not optional. It is standard of care. We must change our practice.
Vinayak Naik
January 15, 2026 AT 07:00Bro, I had this happen to my uncle-he got on lisinopril for ‘borderline’ HTN, creatinine jumped from 1.1 to 3.4 in 9 days. Docs were like ‘oh weird’ and kept going. He ended up in the ER with fluid overload. Turned out he had bilateral stenosis-never knew. Now he’s on amlodipine and doing fine. Just because a drug is ‘common’ doesn’t mean it’s safe. Always check the kidneys first. Seriously. Don’t be that guy.
Saylor Frye
January 15, 2026 AT 18:12Interesting. But I wonder-how many of these cases are actually due to stenosis versus just baseline CKD? The correlation isn’t causation. Also, the ASTRAL trial had major flaws in patient selection. And why are we still using creatinine? It’s outdated. We should be using cystatin C. Also, isn’t this just another example of guideline creep? We’re overmedicalizing a natural aging process.
Kiran Plaha
January 16, 2026 AT 10:31So if I have high blood pressure and I’m 65, should I ask my doctor for an ultrasound before starting any BP med? Is that normal? I’ve never heard of this before. I just want to stay healthy. I don’t want to hurt my kidneys. Can you explain how to ask without sounding like I’m doubting them?