Parasomnia Safety: Understanding Risks, Triggers, and How to Stay Safe
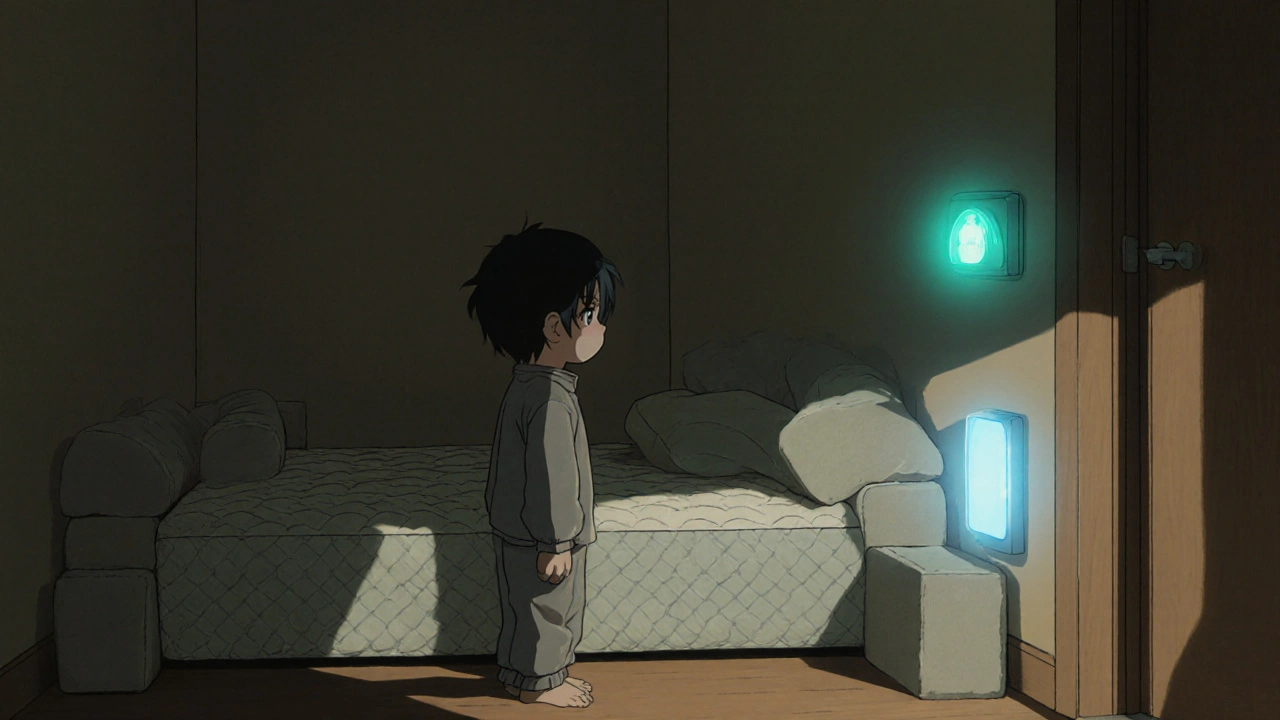
When you or someone you love experiences parasomnia, a group of sleep disorders involving abnormal movements, behaviors, emotions, perceptions, or dreams during sleep. Also known as sleep-related abnormal behaviors, it includes sleepwalking, night terrors, and even sleep-related eating or sex behaviors. These aren’t just strange dreams—they can lead to real injuries, accidents, or dangerous situations if left unaddressed. Unlike normal dreaming, parasomnia episodes happen during deep sleep or the transition between sleep stages, and the person usually has no memory of them afterward. That’s what makes them so risky—you don’t know you’re at risk until something happens.
Many people don’t realize how common and dangerous parasomnias can be. Sleepwalking alone affects up to 4% of adults and even more children. Someone sleepwalking might walk down stairs, leave the house, or even drive a car—without being awake. Night terrors can trigger violent flailing, screaming, or running into walls. These aren’t just scary to watch—they can cause broken bones, head trauma, or worse. That’s why parasomnia safety, the set of practices designed to prevent harm during sleep disorders isn’t optional. It’s essential. And it starts with simple, practical steps: locking windows, removing sharp objects from the bedroom, installing alarms on doors, and keeping the floor clear. Even something as small as placing a gate at the top of stairs can prevent a life-changing fall.
Some triggers are easy to control. Alcohol, sleep deprivation, stress, and certain medications like antidepressants or sedatives can make episodes worse. If you or a family member has frequent episodes, tracking sleep patterns and avoiding these triggers can cut down on incidents. But if episodes are severe, frequent, or involve dangerous behavior, it’s not something to ignore. Medical evaluation might be needed to rule out conditions like epilepsy, PTSD, or other neurological issues. Some people benefit from scheduled awakenings, therapy, or even medication—but only under a doctor’s guidance.
You’re not alone. Millions deal with this quietly, afraid to talk about it. But the truth is, these behaviors are more common than you think—and far more treatable than most assume. The posts below cover real stories, safety checklists, medication risks, and what to do when someone wakes up disoriented or injured during sleep. You’ll find advice on protecting kids, managing adult cases, and recognizing when it’s time to see a specialist. This isn’t about fear—it’s about taking control before something goes wrong.