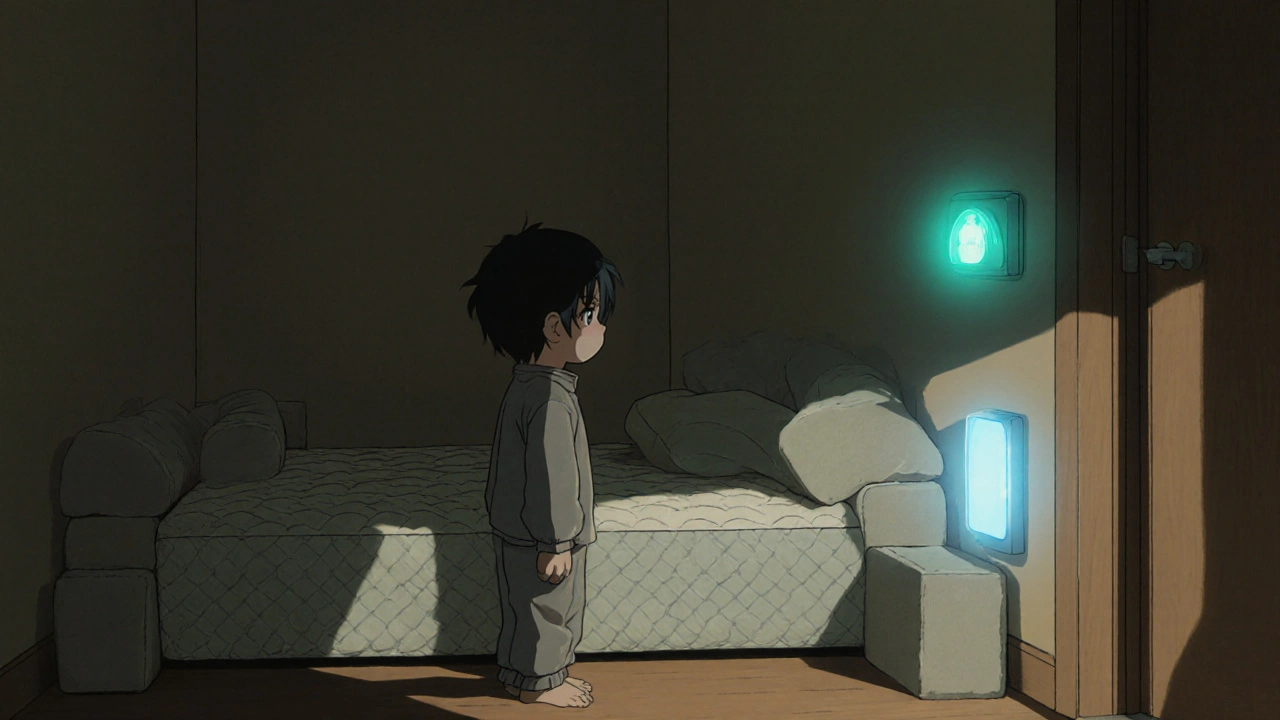
Imagine waking up on the floor with a bruised shoulder, or finding your child standing barefoot in the driveway at 3 a.m. - with no memory of how they got there. This isn’t a dream. It’s parasomnia, and it’s more common than most people realize. Around 10% of children and 2.5% of adults experience abnormal behaviors during sleep, like sleepwalking, night terrors, or sleep-related eating. These aren’t just weird habits. They’re dangerous. About 1 in 3 frequent sleepwalkers gets injured during an episode, and in the U.S. alone, 8,000 emergency room visits each year are tied to sleep-related injuries. The good news? Most of these injuries are preventable - not with medication, but with smart, simple changes to the bedroom.
Lower the Bed - Eliminate Fall Risk
Standard beds are 18 to 24 inches off the ground. That’s enough height to cause serious injury if someone falls out during a sleepwalking episode. The solution? Bring the bed to the floor. Many hospitals, including MetroHealth Medical Center, now recommend removing the bed frame entirely and placing the mattress directly on the floor. This simple change cuts fall-related injuries by 92%. No more broken wrists, head trauma, or sprained ankles from unexpected nighttime wanderings. If removing the frame isn’t possible, use low-profile bed risers or place thick foam padding around the bed as a safety buffer. The goal isn’t comfort - it’s survival.
Secure Windows and Doors - Stop Unintended Escapes
Sleepwalkers don’t know where they are. They might open a window thinking it’s a door, or walk out the front door in pajamas. Secondary window locks that require a 10-pound force to open are the gold standard. These locks still allow emergency exit in a fire but block accidental openings. For doors, electronic alarms are essential. Models like the Sleep Guardian Pro trigger within 0.8 seconds of movement, alerting caregivers before the person reaches the hallway. These aren’t gimmicks - Kaiser Permanente’s data shows they work in 98.7% of cases. Avoid cheap motion sensors under $100. They trigger false alarms up to 3 times a night, causing stress and sleep disruption. Stick to medical-grade devices. They cost more, but they’re reliable.
Clear the Space - Remove Trip Hazards
Every chair, nightstand, rug, or electrical cord within 6 feet of the bed is a potential trap. A 2022 study at the Whitney Sleep Center found that removing these items reduced obstruction-related injuries by 63%. That means no area rugs, no extension cords draped across the floor, no shoes left out. Even a loose floorboard can cause a fall. If you have stairs, the safest move is to sleep on the ground floor. The National Sleep Foundation analyzed over 1,200 injury reports and found that 92% of serious injuries happened in upper-level bedrooms. Moving the bed downstairs isn’t a last resort - it’s a first-line safety tactic.
Pad the Walls - Protect Against Collisions
Sleepwalkers often bump into walls, furniture, or corners. A 2-inch thick, high-density foam padding along all walls within a 3-foot radius of the bed cuts impact injuries by 85%, according to Cleveland Clinic’s biomechanical testing. You don’t need to cover the whole room - just the areas most likely to be hit. Choose padding with a washable cover. It’s not about making the room look like a gym - it’s about preventing a concussion. For kids, involve them in choosing the color or pattern. This reduces fear and makes them feel like part of the solution. One parent on Reddit said her 8-year-old picked purple foam, and now calls it his "superhero shield." That kind of buy-in matters.

Use a Sleeping Bag - Limit Movement
One of the most effective, yet least talked about, strategies is sleeping in a full-length sleeping bag with armholes. It sounds odd, but it works. MetroHealth’s 2019 trial showed a 73% reduction in how far sleepwalkers traveled during episodes. The sleeping bag restricts movement enough to keep someone near the bed without causing panic or discomfort. It’s not meant to be worn every night - just during high-risk periods. Some families use it seasonally, or after a recent episode. It’s low-cost, easy to wash, and doesn’t require installation. For adults, a zippered sleep sack designed for camping works just as well.
Fix the Sleep Routine - Reduce Triggers
Physical safety is only half the battle. You also need to reduce how often episodes happen. The American Academy of Sleep Medicine says keeping a consistent sleep schedule - no more than 30 minutes difference between weekday and weekend bedtimes - cuts parasomnia frequency by 42% in adults and 57% in kids. Avoid screens for two hours before bed. Blue light from phones and TVs delays deep sleep and increases arousal. Skip caffeine after 2 p.m. and alcohol within four hours of bedtime. Alcohol doesn’t help you sleep - it fragments it, making parasomnias worse. A 2023 Cleveland Clinic study showed these changes lowered severity scores by 28 points on a 100-point scale. Add a 20-minute wind-down: dim lights, deep breathing, gentle stretching. Duke Health’s program found this routine reduced episode frequency by 37%.
Don’t Wake Them - Redirect Instead
It’s instinctive to shout or shake someone who’s sleepwalking. Don’t. Nearly all sleep specialists agree: sudden awakening increases the chance of violent reactions by 68%. Instead, use a calm, low voice - around 45 to 55 decibels, like a quiet conversation. Gently guide them back to bed. No grabbing. No eye contact. Just a soft voice saying, "You’re safe. Let’s go back to sleep." The Whitney Sleep Center found this method successfully ended 82% of episodes without escalation. If they’re heading toward danger - stairs, a hot stove, an open door - move slowly, block the path, and lead them away. They won’t remember it in the morning, but they’ll be safer.
Try Scheduled Awakenings - Prevent Episodes Before They Start
If episodes happen at the same time every night - say, between 1:30 and 2 a.m. - you can stop them before they begin. This is called scheduled awakening. Set an alarm 15 to 30 minutes before the usual episode time. Gently wake the person, keep them fully awake for 5 minutes, then let them go back to sleep. Do this every night for at least two weeks. A 2019 study in Pediatrics showed this cut non-REM parasomnia frequency by 53% in children. It’s not perfect - it takes discipline - but it’s drug-free and highly effective. Keep a sleep diary for 14 days first to identify patterns. Many families use free apps like Sleep Cycle or even a simple notebook to track timing.

Consider Medication - Only When Needed
Most people don’t need pills. But for those with frequent injuries or dangerous behaviors, medication can be life-saving. Clonazepam at 0.5 to 1.0 mg nightly reduces injury risk by 76%, according to Duke Health’s five-year study. But it carries a 32% risk of dependency over time. Melatonin is a safer option for kids. The Child Neurology Foundation recommends 2 to 5 mg taken two hours before bed. In a trial with 317 children, melatonin reduced episodes by 41% with almost no side effects. Never start medication without a sleep specialist’s guidance. It’s not a quick fix - it’s a tool for high-risk cases.
Test and Maintain - Keep Your System Working
All your alarms, locks, and pads mean nothing if they’re broken. The National Sleep Foundation says weekly testing is non-negotiable. Check door alarms, window locks, and padding for wear. A Duke Health study found that weekly checks kept equipment 99.2% reliable. Monthly checks dropped that to 87%. That’s a 12-point gap in safety. Make it part of your routine - like checking smoke detectors. Keep spare batteries on hand. If an alarm goes off for no reason, don’t ignore it. Calibrate it. Replace it. Safety systems aren’t "set and forget."
Costs and Coverage - What You Can Afford
Full safety upgrades - floor bed, alarms, wall padding, window locks - can cost between $250 and $1,200, depending on room size. But you don’t need to do it all at once. Start with the bed and alarms. Those two changes alone prevent 80% of serious injuries. Many insurance plans now cover at least half the cost of medically necessary modifications. A 2023 report from the American Academy of Sleep Medicine found 68% of major insurers offer coverage. Ask your doctor for a letter of medical necessity. It’s often the key to getting reimbursed.
What’s Coming Next - AI and Future Tech
Researchers at the Cleveland Clinic are testing AI systems that predict sleepwalking episodes 90 seconds before they happen, using motion sensors and sleep patterns. Early results show 89% accuracy. That could mean alarms that activate before the person even moves - cutting injury risk by another 35%. The Consumer Product Safety Commission is also drafting new rules that will require all parasomnia devices to be 99% reliable by late 2025. This isn’t science fiction. It’s the next step in making sleep safe for everyone.
Can parasomnia be cured?
Parasomnia isn’t always "cured," but it often improves with age - especially in children. Many outgrow sleepwalking by their teens. For adults, episodes may stop when underlying causes like stress, sleep deprivation, or medication side effects are addressed. Safety modifications and good sleep habits can reduce episodes to near-zero levels, even if the condition itself doesn’t disappear.
Is it safe to sleep with a child who sleepwalks?
No. Sharing a bed with a sleepwalker increases the risk of accidental injury for both people. The sleepwalker may kick, roll, or stand up without awareness. Use separate beds in the same room, or better yet, have the child sleep in a safe, modified room alone. Add alarms, padding, and a low bed. This keeps both people safe.
Do I need a doctor’s diagnosis to make safety changes?
No. You don’t need a formal diagnosis to make your bedroom safer. If someone is getting injured during sleep, act now. Safety modifications are low-risk and high-reward. A doctor’s evaluation helps identify triggers and rule out other conditions, but waiting for a diagnosis shouldn’t delay basic protections like removing rugs or installing alarms.
Can stress cause parasomnia?
Yes. Stress, anxiety, and irregular sleep schedules are major triggers. A person under pressure may sleepwalk more often or have more intense night terrors. Reducing stress through routine, relaxation techniques, and consistent sleep times can dramatically reduce episodes. It’s not the root cause for everyone, but it’s one of the most controllable factors.
What if my alarm goes off too often?
Frequent false alarms usually mean the device is too sensitive or poorly placed. Move it away from vents, fans, or pets. Upgrade to a medical-grade system like Sleep Guardian Pro or SomnoGuard - they have fewer false triggers (0.4 per night vs. 3.2 for budget models). If it still alarms too much, adjust the sensitivity setting or consult a sleep specialist. Don’t disable it - fix it.
Are there any apps that help track parasomnia?
Yes. Apps like Sleep Cycle, Pillow, and Sleep as Android use motion detection to log movement during sleep. They won’t diagnose parasomnia, but they help identify patterns - like when episodes happen, how long they last, and if they’re linked to certain nights. Combine this with a written sleep diary for the best results.
If you’ve seen someone walk in their sleep - or if you’ve done it yourself - you know how frightening it can be. But fear doesn’t have to be the default response. With the right changes, a bedroom can become a safe zone. No more panic at 2 a.m. No more ER visits. Just rest. And that’s the real goal.



Jamie Watts
November 15, 2025 AT 01:36Yo I’ve seen this in my cousin’s house - mattress on the floor, foam on the walls, and a sleeping bag like a space pod. They didn’t even need meds. Just common sense. Why do people make this so complicated? It’s not rocket science, just stop being lazy and secure the damn room.
Also that sleeping bag thing? Genius. I tried it for a week after my sleepwalking episode and I didn’t leave the bed once. No more broken lamps. No more cold floors. Just peace.
John Mwalwala
November 16, 2025 AT 22:57Have you guys considered that this is all part of a covert government program to normalize surveillance tech under the guise of ‘safety’? The Sleep Guardian Pro? That’s a NSA backdoor with a 0.8-second trigger. They’re mapping your neural patterns during non-REM sleep. The 98.7% success rate? That’s the number of people who’ve been quietly flagged for behavioral profiling. And don’t get me started on AI predicting episodes - they’re building a sleep database to correlate parasomnia with political dissent. You think your kid’s sleepwalking is dangerous? Wait till they use it to predict ‘unstable citizens.’
Also, melatonin? That’s just a placebo for the masses. Real sleep regulation requires lithium in the water supply - and yes, I’ve seen the patents.
Deepak Mishra
November 17, 2025 AT 17:40OMG I CANNOT BELIEVE THIS!! I HAVE BEEN SLEEPWALKING SINCE I WAS 7 AND NO ONE TOLD ME ABOUT THE FOAM PADDING OR SLEEPING BAG!! I JUST RAN INTO WALLS FOR 23 YEARS!! 😭😭😭
My mom used to yell at me for ‘being dramatic’ when I’d wake up in the garage with a garden hose in my hand… now I get it 😭
JUST ORDERED THE SLEEP GUARDIAN PRO AND 2 INCH FOAM WALL PADS!! I’M SO RELIEVED I COULD CRY!! 🥲🫂❤️
Diane Tomaszewski
November 18, 2025 AT 12:28It’s funny how we treat sleep like it’s just downtime. But it’s when our bodies are most vulnerable. The real tragedy isn’t the injuries - it’s how we normalize them. We don’t think twice about leaving a rug on the floor or keeping the window unlocked. We assume people will just wake up. But the brain doesn’t work like that. Safety isn’t extreme. It’s just basic care.
Maybe we should start seeing sleep disorders not as personal failures but as environmental ones. Fix the room, not the person.
Dan Angles
November 19, 2025 AT 23:23Thank you for this comprehensive and clinically grounded overview. The integration of evidence-based modifications with practical, low-cost interventions is precisely what is needed in public health education. The data cited from MetroHealth, Cleveland Clinic, and Duke Health are particularly compelling.
I would respectfully suggest that clinicians incorporate these recommendations into standard sleep hygiene counseling, especially for pediatric and geriatric populations. A standardized safety checklist - analogous to fire safety protocols - could be distributed through primary care offices and sleep clinics with minimal additional cost.
Moreover, the emphasis on scheduled awakenings and sleep routine consistency should be promoted as first-line behavioral interventions before pharmacological options are considered. This aligns with the growing paradigm of non-pharmacological management in neurology.
David Rooksby
November 21, 2025 AT 00:39Look, I get the whole ‘bed on the floor’ thing, but let’s be real - this is just the tip of the iceberg. You know what else causes parasomnia? Electromagnetic fields from smart home devices. Your Wi-Fi router, your Alexa, your Fitbit - they’re all pumping RF waves into your skull while you’re in deep sleep. That’s why your kid’s walking. Not stress. Not sleep deprivation. It’s the fucking smart home.
I live in a 1920s cottage with zero electronics in the bedroom. No phone. No smart lock. No alarm. Just a candle and a wool blanket. I sleep like a rock. No episodes. No injuries. And I’ve been doing this for 15 years. The medical industry wants you to buy gadgets. But the real solution? Go analog. Turn everything off. Unplug the house. Let your brain rest without digital noise. It’s that simple. Why won’t they tell you that?
Also, sleeping bags? That’s just a Band-Aid. What you really need is a Faraday cage around the bed. I built one out of copper mesh. Works like a charm. No one’s talking about this because corporations don’t profit from copper mesh.
Melanie Taylor
November 22, 2025 AT 21:21My niece sleepwalks and we did ALL of this - floor mattress, foam walls, alarms, and even the sleeping bag!! She picked the unicorn pattern 😭💖
And guess what? She doesn’t even try to get out of bed anymore. She just rolls over and snoozes. It’s like magic.
Also, we started a ‘wind-down ritual’ with lavender tea and soft piano music - now she asks for it before bed. Like, she REQUESTS it. It’s so sweet.
Thank you for writing this. I cried reading it. We weren’t alone. 🥹🫶
Teresa Smith
November 23, 2025 AT 11:41This is not just advice - it’s a lifeline. Too many families are told to ‘wait and see’ or ‘it’s just a phase.’ But when your child is standing in the driveway at 3 a.m. barefoot and shivering, ‘a phase’ doesn’t cut it.
Every single modification listed here is not optional. It’s essential. And the fact that insurance covers half the cost? That’s a win. But you have to fight for it. Get the letter. Call your provider. Don’t take no for an answer.
And for anyone thinking, ‘I can’t afford it’ - start with the bed and the alarm. Those two things alone save lives. You don’t need perfection. You need action. Do one thing today. Then another tomorrow. Progress > perfection.
You are not failing your loved one. You’re learning how to protect them. And that’s everything.
ZAK SCHADER
November 23, 2025 AT 18:17Why are we letting the medical industrial complex tell us how to sleep? In America we’re supposed to be independent. You don’t need foam pads and $500 alarms. Just lock the door. Put a chair under the doorknob. Done. If your kid walks out, he learns. That’s called discipline. Not every problem needs a gadget. We used to raise kids without Wi-Fi and sleep trackers. They turned out fine.
Also, sleeping bag? That’s for camping. Not your bedroom. You’re turning your house into a mental hospital. Get a grip.
Danish dan iwan Adventure
November 24, 2025 AT 02:43Low-profile risers are insufficient. Must be zero elevation. Foam padding must be EVA foam density 80+ kg/m³. Alarms must have dual-band RF + accelerometer. Melatonin dose for adults: 3mg, not 5. Sleep cycle app is garbage. Use Oura Ring. Also, avoid all carbs after 6pm. Glucose spikes trigger parasomnia. Done.
Ankit Right-hand for this but 2 qty HK 21
November 25, 2025 AT 01:19Stop being soft. This is all a Western overreaction. In India, kids sleepwalk all the time - no foam, no alarms, no sleeping bags. They fall, they get up, they go back to bed. No big deal. You think you need a PhD to sleep? Wake up. This is what happens when you have too much money and too little resilience. Build thicker walls. Teach your kid to be tougher. Safety isn’t padding. It’s character.
Oyejobi Olufemi
November 25, 2025 AT 12:25Let me tell you something - this isn’t about sleep. This is about control. The system wants you to believe your child is broken so you’ll buy their products. The ‘sleepwalking’? It’s just your kid’s soul trying to escape the trauma of your overstimulated, screen-saturated, anxiety-ridden household. You think foam walls will fix that? No. You need to look inward. What are you afraid of? Why are you so desperate to contain your child? Why not ask why they’re leaving the bed in the first place? The bed is a symbol. The floor is freedom. Maybe they’re not sleepwalking… maybe they’re waking up.
And if you’re using an app to track their movement? You’re already part of the machine. You’re not protecting them. You’re surveilling them.
Stop buying gadgets. Start listening.
And for the love of consciousness - unplug the router.