When you take antibiotics, you’re not just killing the bad bacteria causing your infection-you’re also wiping out the good ones living in your gut. This imbalance is why so many people end up with stomach cramps, bloating, or worse-diarrhea that lasts for days. It’s not just uncomfortable; it can make you miss work, delay recovery, or even land you back in the doctor’s office with a Clostridioides difficile infection. That’s where probiotics come in. But not all probiotics are the same, and taking them at the wrong time or with the wrong strain can do more harm than good.
Why Antibiotics Mess With Your Gut
Antibiotics don’t pick and choose. Whether you’re on amoxicillin for a sinus infection or vancomycin for a severe bowel infection, these drugs attack bacteria broadly. Your gut holds trillions of microbes that help digest food, make vitamins, and keep your immune system balanced. When antibiotics wipe out large chunks of this community, harmful bacteria like C. diff can take over. Studies show that up to 30% of people on antibiotics develop diarrhea, and about 1 in 5 of those cases are caused by C. diff. The risk goes up if you’re older, in the hospital, or taking broad-spectrum antibiotics like clindamycin or ciprofloxacin.How Probiotics Help-And Which Ones Actually Work
Not every probiotic supplement will help. The key is strain-specific effectiveness. Two strains have the strongest evidence backing them: Lactobacillus rhamnosus GG and Saccharomyces boulardii CNCM I-745.- L. rhamnosus GG has been shown in over 20 clinical trials to reduce the risk of antibiotic-associated diarrhea by up to 60%. It’s the strain in Culturelle and other popular brands.
- S. boulardii is a yeast, not a bacteria, so it’s not killed by antibiotics. It’s especially effective at preventing C. diff infections, with studies showing a 66% reduction in risk.
When and How to Take Them
Timing matters. Taking probiotics at the same time as your antibiotic can reduce their effectiveness-some of the good bacteria might get killed before they even get to your gut. The best practice? Take your probiotic 1 to 2 hours after your antibiotic dose. This gives the antibiotic time to do its job without interfering with the probiotic. Most studies recommend taking probiotics daily for the entire length of your antibiotic course-and then continuing for another 1 to 2 weeks after you finish. Why? Your gut doesn’t bounce back overnight. Even after the antibiotics are gone, your microbiome needs time to rebuild. Skipping the follow-up period means you might miss out on full recovery.Dosage and Product Quality
The right dose makes a difference. Look for products with 10 billion to 100 billion CFUs (colony-forming units) per serving. That’s the range shown to be effective in clinical trials. Lower doses often don’t work. But here’s the catch: product quality varies wildly. A 2021 ConsumerLab test found that nearly half of probiotic supplements didn’t contain the strains or amounts listed on the label. Some had none of the advertised bacteria at all. To avoid this:- Choose brands with the USP Verified mark-these are independently tested for accuracy.
- Refrigerated products tend to have higher live bacteria counts. Shelf-stable ones can lose potency over time.
- Check the expiration date. Probiotics die off as they age.

The Risks: When Probiotics Aren’t Safe
For most healthy people, probiotics are safe. The most common side effect? A little gas or bloating for the first few days. That usually fades. But there are serious risks for certain groups:- Immunocompromised patients-those on chemotherapy, with HIV, or after organ transplants-can develop bloodstream infections from probiotics. At least 12 cases of probiotic-related bacteremia were reported between 2010 and 2020.
- People with central lines or catheters are at higher risk for infection if probiotic bacteria enter the bloodstream.
- Those with severe pancreatitis should avoid probiotics entirely-studies show increased mortality risk.
What About the Controversy? Do Probiotics Delay Recovery?
In 2018, a small but high-profile study in Cell suggested that taking probiotics after antibiotics might actually delay your gut microbiome’s return to normal. The study followed 21 people and found that those who took probiotics took longer to recover their original bacterial balance than those who didn’t. But here’s the full picture: that study was tiny. Other larger studies-including one with over 8,000 patients-show clear benefits in preventing diarrhea and C. diff. The 2022 ISAPP consensus statement concluded that the benefits outweigh the risks for most people. The delay in recovery seen in that one study might be due to the specific multi-strain formula used, not probiotics in general. More research is needed, but for now, the evidence still supports their use for side effect prevention.Probiotics vs. Other Options
What if you’re at high risk for C. diff and probiotics don’t seem strong enough? Fecal microbiota transplantation (FMT) is more effective-it restores the gut with healthy donor stool and reduces C. diff recurrence by over 80%. But it’s invasive, expensive, and only used in hospitals for severe or recurring cases. Probiotics are much simpler: available over the counter, affordable ($20-$45 a month), and safe for most people. They’re not a cure-all, but they’re the best practical tool most of us have to protect our gut during antibiotic treatment.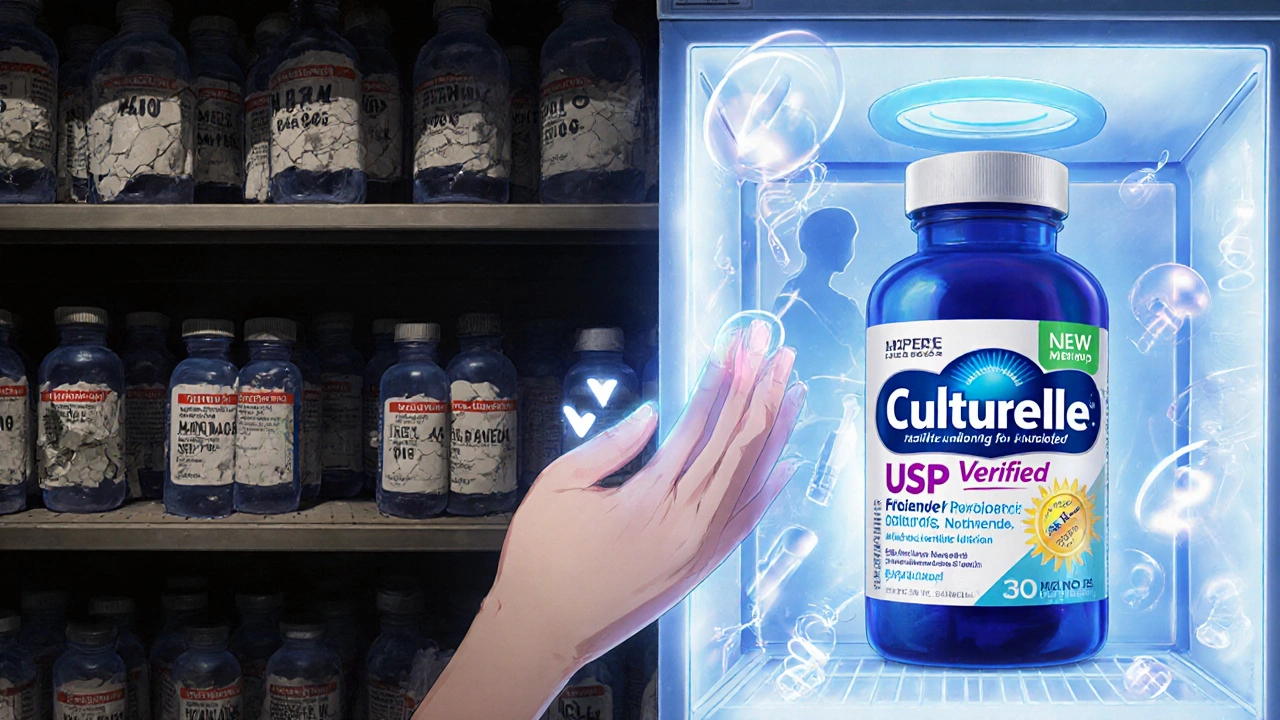
What Experts Say
The Infectious Diseases Society of America (IDSA) recommends probiotics for high-risk patients to prevent C. diff. The American Gastroenterological Association (AGA) is more cautious, citing inconsistent product quality. But most frontline doctors agree: if you’re taking antibiotics and have had diarrhea before, it’s worth trying a proven strain. Dr. Elisa Marroquin, lead author of a major 2022 review, put it simply: “When people take probiotics with antibiotics, we see fewer disruptions to their gut bacteria. Some changes are completely prevented.”What Real People Are Saying
On Reddit and Amazon, users consistently report success:- “Took Culturelle with my amoxicillin and didn’t get a single stomach ache.” - u/MedStudent2023
- “I’ve had diarrhea with every antibiotic until I started S. boulardii.” - Amazon reviewer
- “Spent $35 on Garden of Life and still got C. diff after clindamycin.” - Reddit user
The Future: What’s Coming Next
The probiotic market is booming-worth over $56 billion in 2022. But new concerns are emerging. A 2025 study found that 38% of commercial probiotics carry antibiotic resistance genes. That means the “good” bacteria in your supplement might be hiding genes that help them resist antibiotics-potentially passing those genes to harmful bacteria in your gut. The FDA is now requiring new probiotic products to be screened for these genes. In the next few years, you’ll likely see stricter labeling and fewer untested products on shelves. Meanwhile, next-generation probiotics like VE303-a precise mix of 8 bacterial strains-are showing promise in clinical trials, reducing C. diff by 76%. These aren’t available yet, but they point to a future where probiotics are tailored to your specific antibiotic and microbiome.Final Checklist: What to Do Before Starting
Before you buy a probiotic while on antibiotics, ask yourself:- Am I taking a broad-spectrum antibiotic like clindamycin, ciprofloxacin, or piperacillin-tazobactam? (Higher risk for side effects)
- Do I have a history of antibiotic-associated diarrhea? (Probiotics are most helpful here)
- Am I immunocompromised, on chemotherapy, or have a central line? (Talk to your doctor first)
- Is the product USP Verified or refrigerated? (Avoid unverified, cheap brands)
- Does it contain L. rhamnosus GG or S. boulardii? (Only these two have strong evidence)
- Am I taking it 1-2 hours after my antibiotic? (Timing is critical)
- Will I keep taking it for 1-2 weeks after finishing antibiotics? (Don’t stop too soon)
Can I take probiotics at the same time as my antibiotics?
It’s not recommended. Taking them together can reduce the effectiveness of the probiotic because antibiotics kill bacteria-including the beneficial ones. Wait at least 1 to 2 hours after your antibiotic dose before taking your probiotic. This gives the antibiotic time to work without interfering with the good bacteria.
Which probiotic strain is best for preventing diarrhea from antibiotics?
Lactobacillus rhamnosus GG and Saccharomyces boulardii CNCM I-745 have the strongest evidence. L. rhamnosus GG reduces antibiotic-associated diarrhea by up to 60%, while S. boulardii is especially effective at preventing C. diff infections. Avoid multi-strain products unless they include these specific strains.
Are probiotics safe for everyone?
Most healthy people can take them safely. But if you’re immunocompromised, have a central venous catheter, or have severe pancreatitis, probiotics can cause dangerous infections. Always talk to your doctor before starting if you have a weakened immune system or serious medical condition.
How long should I take probiotics after finishing antibiotics?
Continue for 1 to 2 weeks after your antibiotic course ends. Your gut microbiome takes time to recover, and stopping too soon may mean you don’t get the full benefit. Studies show longer use improves recovery and reduces the chance of recurring issues like diarrhea.
Do all probiotics work the same way?
No. Probiotics are strain-specific. A product labeled "Lactobacillus" could contain dozens of different strains, and only a few have proven benefits. Look for products that list the exact strain name (like L. rhamnosus GG) and have at least 10 billion CFUs per dose. Avoid products without clear labeling.
Why do some people say probiotics didn’t help them?
Several reasons: they used the wrong strain, took too low a dose, didn’t take them at the right time, or bought a low-quality product that didn’t contain live bacteria. Also, probiotics work best for prevention-not for treating an active infection. If you already have diarrhea, probiotics may not reverse it quickly.
Can probiotics cause antibiotic resistance?
Some commercial probiotics carry genes that make them resistant to antibiotics. A 2025 study found 38% of tested products contained antibiotic resistance genes. While the risk of these genes spreading to harmful bacteria is still being studied, the FDA now requires new probiotic products to be screened for these genes. Choose USP Verified brands to reduce this risk.
Is it worth spending more on a high-quality probiotic?
Yes. Cheaper brands often have inaccurate labeling, low bacterial counts, or dead cultures. A $45 USP Verified product with L. rhamnosus GG is far more likely to work than a $10 bottle from a discount store. Your gut health is worth the investment-especially when you’re already taking antibiotics.





Nicole M
November 12, 2025 AT 23:20I took Culturelle with amoxicillin last winter and barely felt a thing. My last course without it was a disaster-three days of cramps and panic attacks every time I left the house. Just stick to L. rhamnosus GG and wait two hours after your pill. It’s not magic, but it’s the closest thing we’ve got.
Arpita Shukla
November 14, 2025 AT 00:59Actually, the 2018 Cell study you mentioned is the most important one here. The gut microbiome doesn’t need external help to recover-it’s self-regulating. Probiotics are just transient visitors. Most people who claim they work are just experiencing placebo or natural recovery. The real issue is overprescribing antibiotics in the first place.
Mark Rutkowski
November 15, 2025 AT 11:24There’s something beautiful about the idea that our bodies are ecosystems-wild, complex, and deeply interconnected. Antibiotics are like a wildfire. Probiotics? They’re not a fire extinguisher. They’re more like planting seeds in the ash, hoping something green will grow. And sometimes, it does. Sometimes, it doesn’t. But isn’t that the whole point of life? We don’t control the storm-we just learn how to dance in it. And maybe, just maybe, a little L. rhamnosus GG helps us find the rhythm again.
Ryan Everhart
November 17, 2025 AT 11:03So let me get this straight-you’re telling me to spend $45 on a pill that might not even have the bacteria it claims to have… but I should trust the USP label? Meanwhile, my grandma fermented cabbage in a jar for $0.50 and never once got diarrhea. Also, why are we treating gut health like it’s a tech upgrade? You don’t need a new OS to fix a broken keyboard.
David Barry
November 18, 2025 AT 10:55Let’s be real: 80% of probiotic users are middle-class Americans who’ve been sold a dream by Big Wellness. The data is messy. Some studies show benefit. Others show delay. The only consistent thing? Profit margins. And let’s not forget-most of these trials are funded by supplement companies. The real breakthrough? Stopping antibiotics unless absolutely necessary. That’s the only intervention with a 100% success rate: not taking them.
Alyssa Lopez
November 20, 2025 AT 05:36USP VERIFIED IS A JOKE. I bought a bottle labeled '100 Billion CFU' and it was just sugar and fillers. I'm not some hippie-I'm a nurse. I've seen C. diff in ICU. Probiotics are legit. But you gotta go with the real stuff-S. boulardii. No excuses. And yeah, take it after the abx. DUH. Also, stop buying from Walmart. They sell expired probiotics like candy. #GutHealth #NoMoreCheapSupps
Alex Ramos
November 21, 2025 AT 00:32For real-this post is gold. I’ve been giving S. boulardii to my patients on clindamycin for years. One guy had 3 C. diff episodes before we started him on it. Now he’s fine. Just make sure it’s refrigerated and check the date. And yeah, timing matters. I tell people: take your antibiotic at 8am, probiotic at 10am. Simple. Also-yogurt doesn’t cut it. Too few CFUs. Stick to the science. 🙌