Lithium Drug Interactions: What You Need to Know Before Taking It
When you take lithium, a mood-stabilizing medication primarily used to treat bipolar disorder. Also known as lithium carbonate, it works by balancing brain chemicals—but it’s not forgiving when mixed with other drugs or even common supplements. Unlike many medications, lithium has a very narrow safety window. Too little won’t help. Too much can be dangerous. That’s why understanding lithium drug interactions isn’t optional—it’s life-saving.
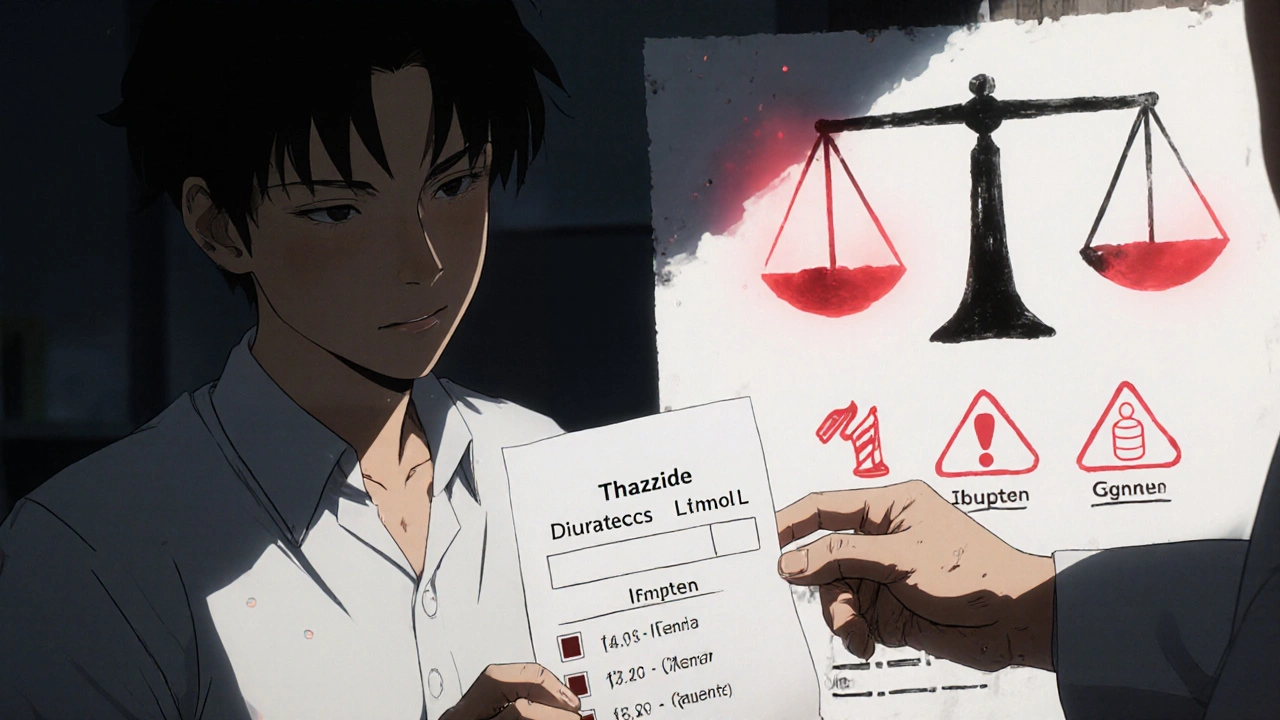
Lithium doesn’t just react with other pills. It’s heavily affected by your body’s fluid balance. Diuretics (water pills), common for high blood pressure, can cause lithium to build up in your system. Even over-the-counter NSAIDs like ibuprofen or naproxen can raise lithium levels, increasing the risk of toxicity. If you’re on lithium and start taking any new medication—even for a headache or allergy—you need to tell your doctor. The same goes for salt intake. Suddenly eating much less salt (like on a strict diet) or much more (like from processed foods) can throw off your lithium levels. Your kidneys are the main way your body gets rid of lithium, so anything that stresses them—dehydration, kidney disease, or certain antibiotics—can be risky.
Thyroid and kidney health are closely tied to lithium use. Many people on long-term lithium develop hypothyroidism, which means their thyroid doesn’t make enough hormone. That’s why regular blood tests for thyroid function aren’t just routine—they’re essential. Kidney function also needs checking every few months. If your kidneys slow down, lithium stays in your body longer. Some people develop mild kidney changes over years, but catching it early means you can adjust your dose or switch treatments before it becomes serious.
What about other mood stabilizers? If lithium isn’t working or causes too many side effects, alternatives like lamotrigine, a mood stabilizer often used for bipolar depression or valproate, a seizure and mood stabilizer with different interaction risks might be better options. These don’t require the same level of blood monitoring as lithium, but they come with their own set of concerns—like liver health or birth defects. The point isn’t to avoid lithium, but to use it wisely. Many people live well on it for decades, as long as they stay on top of checkups and avoid risky combos.
There’s no magic trick to avoiding lithium interactions. It’s about consistency: take your dose at the same time each day, drink enough water, avoid sudden diet changes, and never start or stop another medication without talking to your provider. Keep a simple list of everything you take—prescription, OTC, herbs, vitamins—and bring it to every appointment. If you feel shaky, nauseous, confused, or notice unusual muscle weakness, don’t wait. Those could be early signs of lithium toxicity. Get checked right away.
Below, you’ll find real-world guides that break down how lithium compares to other mood stabilizers, what to watch for in daily use, and how to spot dangerous interactions before they hurt you. These aren’t theoretical—they’re written by people who’ve been there, and they focus on what actually matters when you’re managing your health every day.