When you have rheumatoid arthritis (RA), knowing how active your disease is isn’t just about how sore your joints feel. It’s about making smart, timely decisions that stop damage before it happens. That’s where tools like CDAI, DAS28, and imaging come in. These aren’t just numbers on a chart-they’re your roadmap to remission, fewer flare-ups, and keeping your hands, knees, and wrists working longer.
What CDAI Tells You (And Why It’s Becoming the Standard)
The Clinical Disease Activity Index, or CDAI, is a simple, no-lab-needed way to measure RA activity. It adds up four things: the number of tender joints (out of 28), swollen joints (also out of 28), how you rate your overall symptoms on a scale of 0 to 10, and how your doctor rates them. That’s it. No blood tests. No waiting for results. Just a quick count and a few questions.
That simplicity is why CDAI is now used in 78% of U.S. rheumatology practices-up from just 45% in 2015. It fits into a 2-minute check-in. Most electronic health records even calculate it automatically. A score under 2.8 means you’re in remission. Between 2.8 and 10? Low disease activity. Over 22? That’s high activity, and it’s time to change your treatment.
Studies show CDAI is one of the best predictors of joint damage. People with scores above 22 are over four times more likely to develop new erosions within a year than those in remission. It’s not perfect-it doesn’t measure inflammation directly-but it’s incredibly reliable at spotting real-world disease impact. Doctors trust it because it lines up closely with how they see patients in person. In fact, one 2023 study found CDAI matched physician judgment better than any other score.
DAS28: The Inflammation Tracker That Needs a Lab
DAS28 is the older sibling of CDAI. It also uses tender and swollen joints-but adds blood markers. There are two versions: DAS28-ESR (uses erythrocyte sedimentation rate) and DAS28-CRP (uses C-reactive protein). Both give you a more complete picture of inflammation inside your body.
The formula looks complicated, but you don’t need to do the math. Your doctor’s office does. A score under 2.6 is remission. Between 2.6 and 3.2? Low activity. Above 5.1? High activity. DAS28 is great when you need to know if your body is still fighting inflammation, even if your joints don’t feel swollen. That’s why it’s still the top choice in Europe, used in 68% of practices there.
But here’s the catch: you have to wait for lab results. In 68% of cases, doctors say the CRP or ESR results come in after the appointment. That means they have to guess your score and adjust treatment later. Some patients feel frustrated when their treatment changes because of a blood test they didn’t even know was done.
DAS28-CRP is becoming more popular than DAS28-ESR because CRP rises and falls faster than ESR. That means it can catch a flare sooner. But if your clinic doesn’t have fast lab turnaround, CDAI often wins out for day-to-day use.
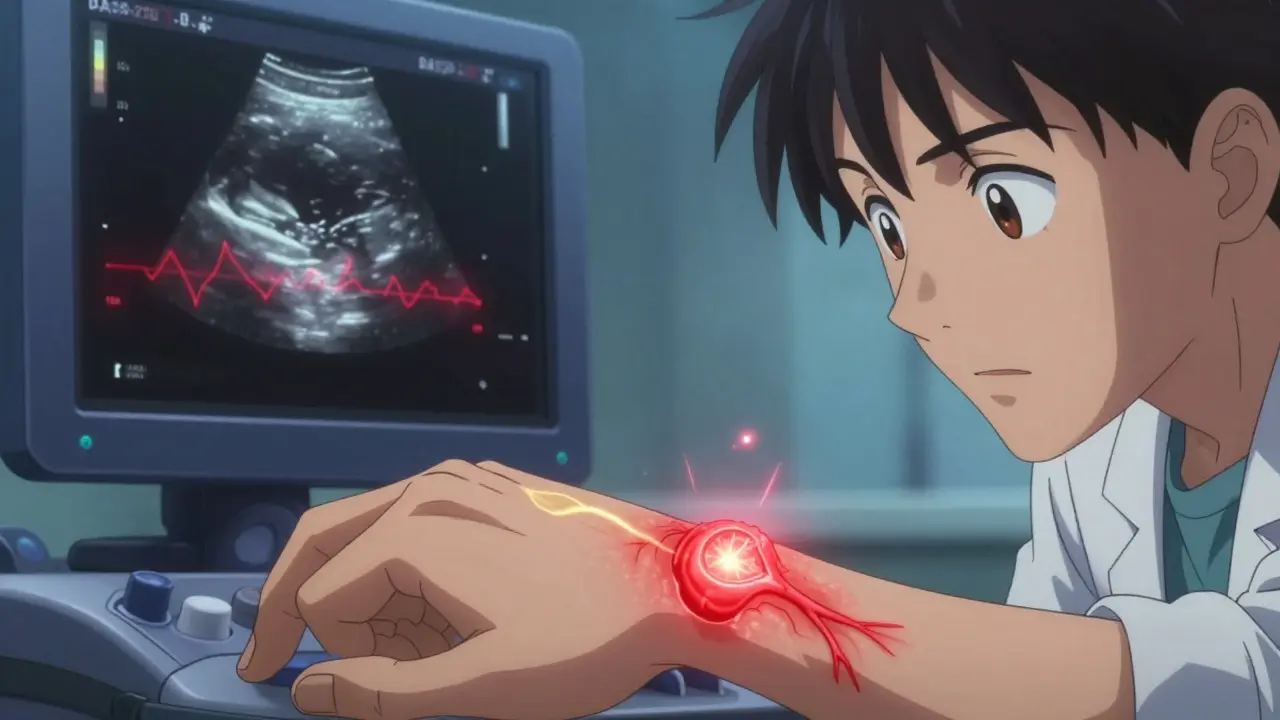
Imaging: Seeing What Your Eyes Can’t
Two things happen in RA that you can’t feel: bone erosion and synovitis (inflamed joint lining). Clinical exams miss these early. That’s where imaging steps in.
Conventional X-rays have been the gold standard for decades. They show bone damage-holes, narrowing, deformities. But they’re slow. It can take 6 to 12 months before damage shows up on an X-ray. By then, it’s already happened. Still, they’re cheap, widely available, and perfect for tracking long-term damage over years. The Sharp/van der Heijde scoring system rates damage across 44 joints. A yearly increase of 5 points or more means your disease is actively destroying tissue.
Ultrasound is changing the game. It can see swollen synovium and extra blood flow (power Doppler) before joints get hot or swollen. It’s fast, non-invasive, and costs about $150-far less than an MRI. In 63% of U.S. rheumatology visits today, ultrasound is used. When a doctor sees synovitis on ultrasound but no swelling on exam, they change treatment in 22% of cases. Patients love it too. Seeing the inflammation on screen makes it real. One patient said, “I finally understood why I needed a new drug-it wasn’t just in my head.”
MRI is the most sensitive tool. It spots bone edema-fluid in the bone that happens before erosion. Studies show 89% of people with bone edema on MRI will develop erosions within a year. That’s why it’s used in clinical trials and specialized centers. But it’s expensive ($1,200 per scan in the U.S.) and not practical for routine use. Most doctors reserve it for unclear cases or high-risk patients.
When to Use What? A Practical Guide
There’s no one-size-fits-all. Here’s how most experts combine these tools:
- Every visit: Use CDAI. It’s fast, reliable, and tells you if your treatment is working in real life.
- Every 3-6 months: Add DAS28-CRP if inflammation is suspected or if you’re not improving on CDAI alone.
- When things are unclear: Order ultrasound. If your joints feel okay but your score is high, ultrasound can show hidden inflammation.
- For new diagnosis or rapid progression: Use MRI to check for early bone damage. If you’ve had RA for less than a year and your joints are hurting badly, an MRI can catch damage before X-rays can.
- Once a year: Get an X-ray to track long-term structural damage. This helps judge if you’re preventing erosion over time.
Some clinics now use hybrid approaches. The NIH-funded RACoon trial is testing a system that combines CDAI scores, ultrasound results, and wearable activity trackers. The goal? Personalize monitoring. If your score stays low and your movement data looks normal, you might only need a check-up every six months. If your score spikes and your steps drop, you get an ultrasound right away.
What Patients Say About Monitoring
Patients have strong opinions. In a 2023 survey of nearly 3,000 people with RA:
- 68% prefer filling out symptom apps before their appointment-it’s easier than remembering how they felt last week.
- 42% feel anxious when they know their self-reported pain will affect treatment decisions.
- 52% feel pressured to get MRIs they don’t need.
- 38% appreciate ultrasound because they see the inflammation during the visit-no waiting for reports.
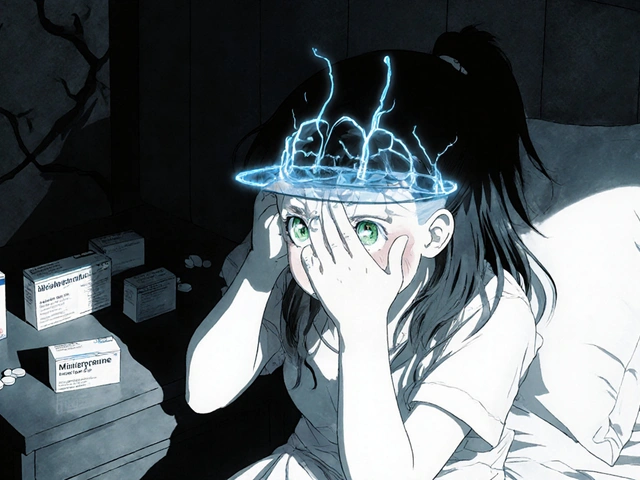
There’s also a big gap between what patients and doctors see. In one Brazilian study, 33% of patients rated their pain higher than their doctor did. That doesn’t mean they’re exaggerating. It means pain and inflammation don’t always match. Doctors focus on joint counts and lab results. Patients feel fatigue, stiffness, and mental fog-things CDAI and DAS28 don’t fully capture.
That’s why experts now say: don’t rely only on scores. Ask about sleep, energy, and mood. Fatigue alone accounts for 14% of what patients consider a meaningful improvement. If your score says remission but you’re still exhausted, your treatment isn’t done.
Challenges and What’s Next
Even with all these tools, problems remain. Inter-rater reliability is a big one. Two doctors counting the same 28 joints can get different results. That’s why training matters. Fellowship programs now use standardized videos to teach joint counting. After 10 supervised sessions, reliability jumps to 85-90%.
Another issue: 22% of U.S. rheumatology practices still don’t use any standardized score. Many are small, rural clinics without the resources or training. That’s a gap in care.
Technology is closing that gap. New software like QUASAR can automatically analyze ultrasound images with 88% accuracy. The ACR’s new “RA Monitor” EHR module auto-triggers imaging referrals when CDAI hits 10 or higher. AI tools are being trained to spot erosions on X-rays and MRIs with 92% accuracy.
By 2027, experts predict half of RA monitoring will include remote data-wearables tracking movement, sleep, and heart rate-combined with clinic visits. The future isn’t just about numbers on a screen. It’s about continuous, real-time data that adapts to your life.
Final Takeaway: Monitoring Is Your Shield
Rheumatoid arthritis isn’t just about pain. It’s about slow, invisible damage that can steal your independence. CDAI gives you a clear, daily snapshot. DAS28 tells you if inflammation is still burning inside. Imaging shows you what’s happening under the skin-before it’s too late.
Using these tools together isn’t about being overly medicalized. It’s about taking control. If you’re in remission, you can reduce meds. If you’re not, you can switch faster. Studies show this approach cuts joint damage by 30-50% compared to old-school care.
Ask your doctor: Which score do you use? When do you order imaging? Do you check for fatigue? If they can’t answer, it’s time to find a provider who does. Your joints are counting on it.




Cara C
December 21, 2025 AT 04:26I’ve been using CDAI for over a year now, and honestly? It’s been a game-changer. No more waiting for labs, no guesswork. I fill out my joint count and pain score on my phone before each visit, and my rheum just pulls it up. It feels like I’m actually part of the decision-making, not just a patient checking a box. Plus, seeing my score drop from 18 to 1.5? That’s motivation to keep going.
My doctor even started using it for my mom too-she’s 72 and hates blood draws. This way, she gets care without the stress.
It’s not perfect, but it’s real. And that matters.
Michael Ochieng
December 22, 2025 AT 07:09Just came back from Nigeria last month and talked to a few rheumatologists in Lagos. They’re still mostly using DAS28-ESR because CRP kits are expensive and ESR tubes are cheaper. But they’re starting to adopt CDAI too-especially in rural clinics where labs take 3 days to come back.
One doc told me he trains nurses to count joints using a tablet app. He said, ‘If you can’t measure it, you can’t manage it.’ And honestly? That’s the truth. We need tools that work where people live, not just where the labs are fast.
Also, ultrasound is slowly creeping in. One hospital bought a portable machine last year. Patients cry when they see the inflammation on screen. It’s not just numbers anymore-it’s real.
Dan Adkins
December 22, 2025 AT 14:57It is regrettable that the article fails to address the fundamental limitations of CDAI in populations with comorbidities such as fibromyalgia or chronic pain syndromes. The subjective nature of patient-reported outcomes renders the index statistically unreliable in such cohorts. Moreover, the uncritical adoption of CDAI in 78% of U.S. practices reflects a dangerous trend toward procedural standardization at the expense of clinical nuance.
One must also consider the cultural bias inherent in the 0–10 pain scale. In certain non-Western populations, pain expression is culturally moderated, leading to underreporting. This is not a flaw in the patient-it is a flaw in the metric.
Furthermore, the assertion that CDAI ‘matches physician judgment better than any other score’ is not substantiated by robust multicenter validation. The referenced 2023 study had a sample size of 127 patients. That is not generalizable. The author’s tone suggests an uncritical embrace of American-centric protocols without acknowledging global heterogeneity in care delivery.
Erika Putri Aldana
December 23, 2025 AT 14:37why do we need 4 different scores to know if our joints suck??
i just want to not cry when i open a jar
also why is everyone so obsessed with numbers when i feel like a ghost most days??
Grace Rehman
December 25, 2025 AT 06:26So we’re measuring inflammation with blood tests and joint counts… but still treating fatigue like it’s a side effect of being sad?
Let me get this straight-you can have a CDAI of 1.2, zero swollen joints, CRP normal… and still be too exhausted to brush your teeth. And yet, your doctor says you’re in remission.
Remission from what? The pain? Or the part of your life that made you you?
I don’t need another algorithm. I need someone to ask if I slept. If I cried before my appointment. If I still feel like a person.
And no, I’m not ‘overreacting.’ I’m just tired of being measured like a lab sample.
Also-why is it always the patient’s job to advocate for the things that matter? Why isn’t the system built around that?
Jerry Peterson
December 26, 2025 AT 19:12Had a weird moment last week-my rheum pulled up my CDAI and said, ‘You’re in remission.’ I said, ‘But I can’t lift my coffee cup.’ He paused, looked at me, and said, ‘Then we’re missing something.’
He ordered an ultrasound on the spot. Found synovitis in my wrist. Changed my med. Two weeks later, I’m back to making pancakes.
Point is: scores are tools, not verdicts. If you feel off, push back. Even if the number says you’re fine. Your body doesn’t lie just because the chart does.
Meina Taiwo
December 27, 2025 AT 07:02Ultrasound is the real MVP. Saw synovitis in my knee when no one else could feel anything. Changed my whole treatment. Worth every penny.
Orlando Marquez Jr
December 28, 2025 AT 10:47The assertion that CDAI is now used in 78% of U.S. rheumatology practices requires citation of a peer-reviewed national survey. The figure cited appears to be extrapolated from a single regional study conducted in 2022. Without transparent sourcing, such statistics risk misleading clinicians and patients alike. Furthermore, the claim that CDAI ‘matches physician judgment better than any other score’ lacks methodological context-was this assessed via inter-rater reliability? Concordance with imaging? Long-term outcomes? Without this, the statement remains anecdotal.
Jon Paramore
December 29, 2025 AT 07:04Let’s not forget the biologic half-life factor. CDAI and DAS28 are snapshots, but disease activity is dynamic. If you’re on a biologic with a 14-day half-life, a single CDAI score at week 4 tells you nothing about trough levels or subclinical flare risk. That’s why we combine it with CRP trends and serial ultrasound-especially in early RA. The real innovation isn’t the tool-it’s the longitudinal integration. AI-driven predictive modeling based on CDAI + wearables + CRP trends is already showing 89% accuracy in predicting flares 30 days out in the RACoon pilot cohort. This isn’t the future. It’s Q3 2024.