Bacterial Mutations: How Drug Resistance Develops and What It Means for Your Health
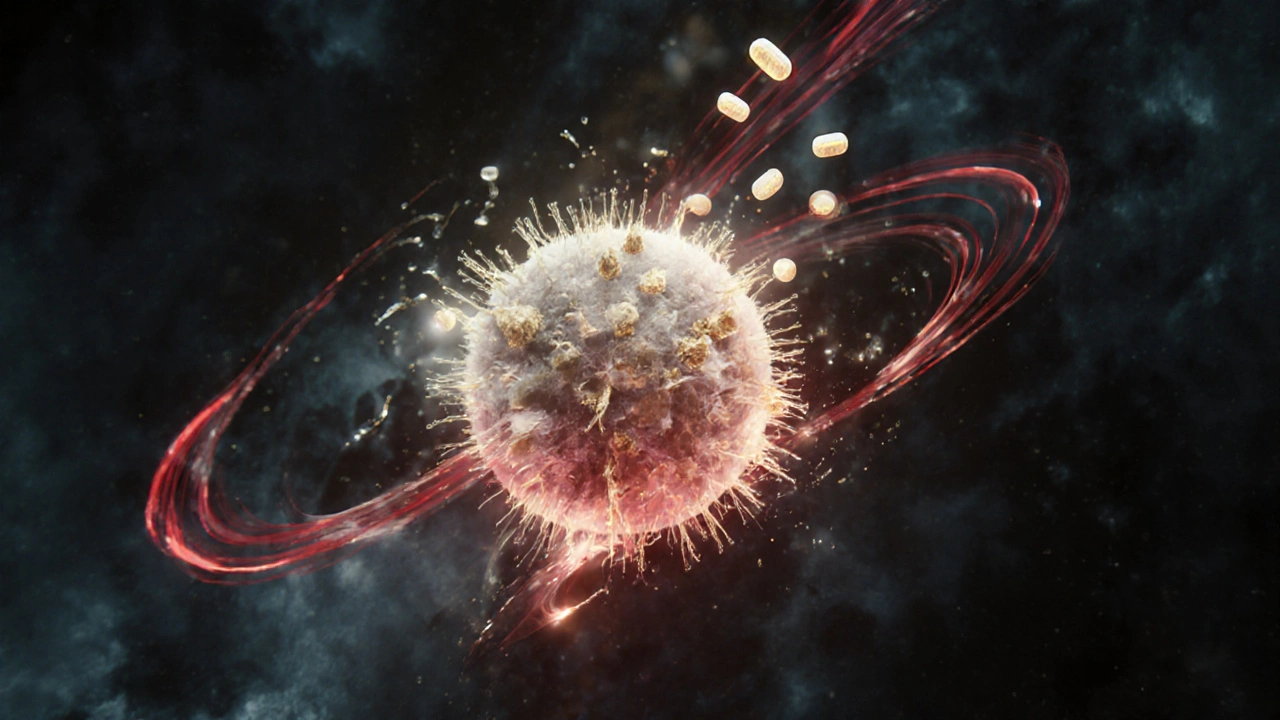
When we talk about bacterial mutations, random changes in a bacterium’s DNA that can alter how it behaves, grows, or responds to drugs. Also known as genetic drift in microbes, these changes are natural—but when they help bacteria survive antibiotics, they become dangerous. Every time you take an antibiotic, you’re not just targeting the bad bugs—you’re giving the ones with the right mutations a survival advantage. That’s how antibiotic resistance, the ability of bacteria to withstand drugs designed to kill them starts. It’s not magic. It’s evolution, happening fast, right in your body or in hospitals and farms around the world.
These mutations don’t happen because antibiotics "create" superbugs. They already exist in tiny numbers. Antibiotics just wipe out the weak ones, leaving the tough ones to multiply. Over time, that’s how a harmless strain turns into a drug-resistant bacteria, a strain that no longer responds to standard treatments, forcing doctors to use stronger, riskier drugs. This isn’t just a hospital problem. It shows up in everyday infections—sinusitis, urinary tract infections, even skin wounds. And when one drug stops working, doctors reach for the next. But there’s a limit. The pipeline for new antibiotics is drying up, while mutations keep coming.
Some of these mutations come from overuse—taking antibiotics for viral colds, not finishing a full course, or using them in livestock to speed up growth. Others come from poor sanitation or unregulated drug sales. The result? superbugs, bacteria that resist multiple drugs, sometimes all known treatments like MRSA, VRE, and CRE. These aren’t sci-fi threats. They’re real. People die from infections we used to treat in hours. And the more we rely on antibiotics, the faster these bugs adapt.
What does this mean for you? If you’ve ever had an infection that didn’t clear up with the first round of pills, you’ve seen bacterial mutations in action. It’s why proper dosing matters. It’s why you shouldn’t share or save antibiotics. It’s why some infections now need IV drugs, longer hospital stays, or no cure at all. The good news? We’re learning more every day. Research into how mutations spread, how to block them, and how to use existing drugs smarter is growing. But progress depends on awareness—and action.
In the posts below, you’ll find real-world guides on how medications are used, stored, and monitored to fight back against these threats. From verifying your pills with FDA tools to understanding how antibiotics affect your gut, each article connects to the bigger picture: how we use drugs today shapes the bacteria of tomorrow. You’re not just treating an infection. You’re helping decide which bugs survive.