When you take a new medication, you might expect side effects like a stomach ache or drowsiness. But if your skin breaks out in hives, your throat swells, or you can’t breathe, that’s not a side effect - it’s a drug allergy. Unlike regular side effects, which happen because of how the drug works in your body, a drug allergy means your immune system is fighting the medicine like it’s a virus. And that can turn deadly fast.
What Does a Drug Allergy Actually Look Like?
- Skin rash or hives - red, itchy bumps that come up suddenly. They might spread quickly and feel warm to the touch.
- Itching - not just a little itch. This is intense, widespread, and doesn’t go away with over-the-counter creams.
- Swelling - lips, tongue, eyelids, or throat. If your throat swells, you might feel like you’re choking, even if you haven’t eaten anything.
- Difficulty breathing - wheezing, coughing, or feeling like your airway is closing. This is a major red flag.
- Low blood pressure - dizziness, fainting, or sudden weakness. You might feel cold and clammy.
- Gastrointestinal issues - vomiting, diarrhea, or cramps that come on fast after taking the pill.
- Fever and swollen lymph nodes - if these show up days or weeks later, it could be a delayed reaction like DRESS syndrome.
Here’s the thing: not all rashes are allergies. A mild, slow-developing rash that appears after a few days and doesn’t come with other symptoms might just be a side effect. But if you get two or more of those symptoms together - say, a rash and trouble breathing - that’s anaphylaxis. And that’s an emergency.
Timing Matters: When Do Reactions Happen?
Drug allergies don’t always strike right away. The timing tells you a lot about what you’re dealing with.
- Within minutes to an hour - This is the classic IgE-mediated reaction. Think hives, swelling, trouble breathing, or vomiting. Penicillin, sulfa drugs, and certain painkillers like ibuprofen or naproxen often cause this type.
- Days later - A flat, red rash that spreads slowly over your chest or back? It could be a delayed drug exanthem. This is common with antibiotics like amoxicillin or anticonvulsants. It’s usually not life-threatening but still needs a doctor’s eye.
- One to three weeks later - If you develop a fever, swollen glands, joint pain, and a rash, you might have serum sickness-like reaction. It’s rare, but it happens with drugs like cefaclor or some blood pressure meds.
- Weeks to months - DRESS syndrome is the most dangerous delayed reaction. It can damage your liver, kidneys, or lungs. Symptoms include a widespread rash, high fever, swollen lymph nodes, and abnormal blood counts. This requires hospitalization.
That’s why taking pictures of any rash or unusual reaction is a smart move. If you can’t get to a doctor right away, those photos help them spot the pattern.
When to Call 911 - Not Your Doctor
If you have any of these, don’t wait. Don’t call your pharmacy. Don’t check Google. Call 911.
- Swelling in your throat or tongue
- Wheezing or gasping for air
- Feeling like you’re going to pass out
- Confusion or dizziness
- Multiple symptoms at once - rash + breathing trouble + vomiting
This is anaphylaxis. It can kill in under 30 minutes. Emergency responders carry epinephrine, which can reverse the reaction. Hospitals have the tools to stabilize you. Waiting to see if it gets better is a gamble you can’t afford.

What Happens After the Emergency?
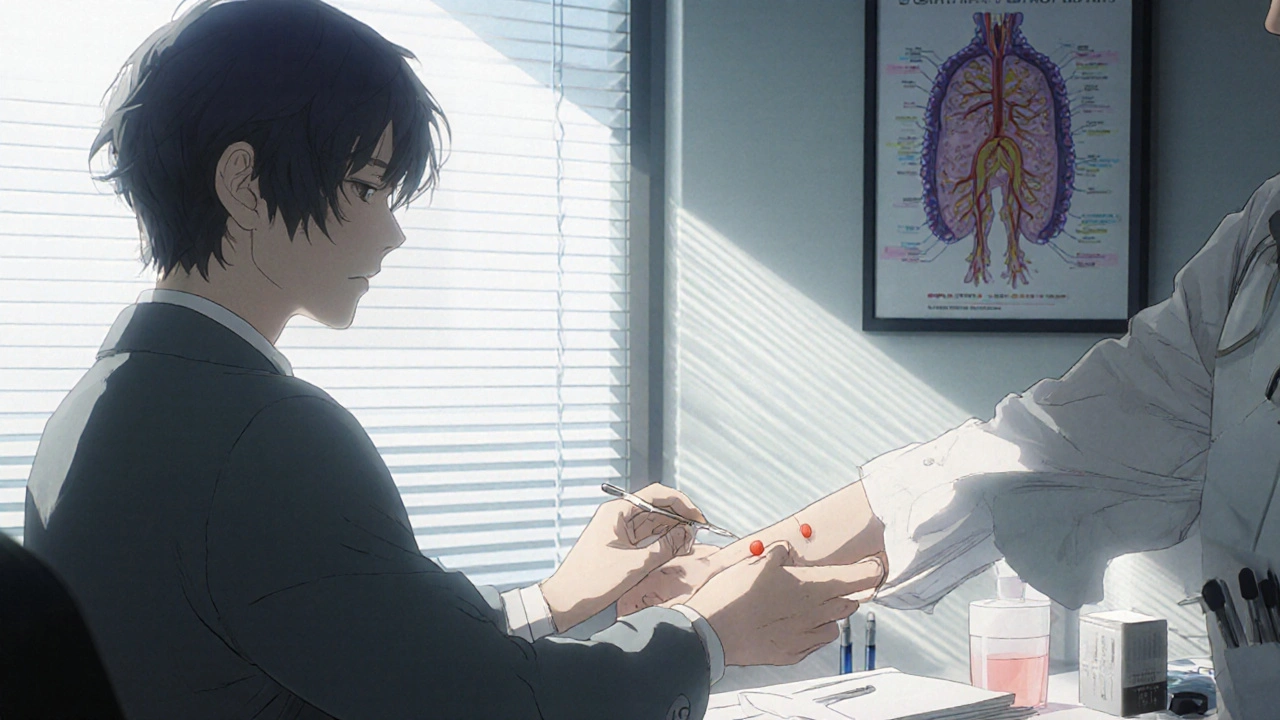
Once you’re stable, you’ll need to see an allergist. Most doctors won’t know how to test for drug allergies - except for penicillin. That’s the only one with a reliable skin test.
For penicillin, the process is straightforward: a tiny prick on your skin with the drug. If you’re allergic, a red bump appears. If not, you might get a small oral dose under supervision to confirm. Studies show over 90% of people who think they’re allergic to penicillin aren’t. They were mislabeled after a childhood rash that wasn’t an allergy. That means they’ve been given worse, more expensive, and riskier antibiotics for years.
For other drugs? Testing is harder. Blood tests can help for severe delayed reactions like DRESS. But for most, the diagnosis comes down to your history - what you felt, when, and how it looked. That’s why writing down every detail matters.
Why Mislabeling Is a Hidden Crisis
One in ten Americans thinks they’re allergic to a drug. But most of them aren’t. The problem? That label sticks in your medical record forever. Doctors avoid prescribing the drug, even if it’s the best option. You might get clindamycin instead of penicillin for a strep throat - and that raises your risk of a deadly gut infection called C. diff. You might get a stronger antibiotic that messes with your gut bacteria, causes diarrhea, or even leads to antibiotic resistance.
It’s not just about you. It drives up costs for the whole system. The NIH says mislabeling leads to higher hospital stays, more ER visits, and longer recovery times. That’s why getting tested isn’t just personal - it’s public health.
What You Can Do Right Now
- Write it down - When you have a reaction, note the drug name, dose, time taken, and all symptoms. Include how long they lasted.
- Take photos - Rashes change fast. A picture is worth a thousand words to a doctor.
- Don’t self-diagnose - Just because your cousin had a rash on amoxicillin doesn’t mean you will.
- Ask for a referral - If you’ve had a serious reaction, ask your primary doctor to refer you to an allergist. Don’t wait until the next time you’re sick.
- Wear a medical alert - If you’ve had anaphylaxis, get a bracelet or app alert that says your allergy. Paramedics need to know fast.
Bottom Line
Drug allergies are rare, but they’re dangerous. The key isn’t avoiding all meds - it’s knowing the difference between a side effect and a true immune reaction. If you feel like your body is shutting down, act immediately. If you’re unsure, see an allergist. And if you’ve been told you’re allergic to penicillin, get tested. You might be able to take it safely again - and that could save your life the next time you’re sick.
Can you outgrow a drug allergy?
Yes, especially with penicillin. Many people who had a rash as a child are no longer allergic as adults. The immune system changes over time. That’s why retesting is important - you might be able to safely use the drug again.
Is a rash always a sign of drug allergy?
No. Many rashes are side effects, not allergies. A slow-developing, non-itchy rash that appears days after starting a drug is often not immune-related. But if it’s itchy, spreading fast, or comes with swelling or breathing trouble, treat it as a possible allergy until proven otherwise.
Can you have an allergic reaction the first time you take a drug?
Yes. Even if you’ve never taken the drug before, your immune system can mistake it for a threat. You don’t need to have been exposed before to have an allergic reaction. The first time can be the worst.
Are there any drugs that cause more allergies than others?
Penicillin and related antibiotics are the most commonly reported. But sulfa drugs, NSAIDs like ibuprofen, chemotherapy drugs, and certain seizure medications also trigger reactions more often. The more you take a drug, the higher your risk - but even one dose can cause a reaction.
What if I’m allergic to one drug - will I be allergic to others?
Not necessarily. Being allergic to penicillin doesn’t mean you’ll react to aspirin or insulin. But some drugs are chemically similar. If you’re allergic to one sulfa drug, you might react to others in the same class. Always tell your doctor about every reaction you’ve had.
Can I take over-the-counter antihistamines for a drug allergy?
Only for mild, isolated symptoms like itching or a small rash - and only after stopping the drug. If you have swelling, trouble breathing, or dizziness, antihistamines won’t help enough. They don’t stop anaphylaxis. Never delay calling 911 because you’re taking an antihistamine.
How do I know if I need to see an allergist?
If you’ve had a reaction that involved more than one body system - like skin + breathing, or rash + vomiting - you should see one. Also, if you’ve been labeled allergic without testing, or if you’ve avoided a drug that’s commonly used (like penicillin), an allergist can help you find out if it’s safe to take again.



Levi Hobbs
November 17, 2025 AT 09:25I had a rash after taking amoxicillin in college-thought it was just a side effect. Turned out it was a delayed exanthem. Took me three months and three doctors to get it figured out. Now I carry a card in my wallet that says 'Amoxicillin: Not a side effect, it's an immune response.' Don't wait like I did. Write it down. Take pictures. Even if it seems minor.
Joseph Peel
November 17, 2025 AT 20:25The distinction between side effect and allergic reaction is critically undercommunicated in primary care. A rash that emerges 72 hours after ingestion, without systemic involvement, is typically a non-IgE-mediated drug eruption-not an allergy. Misclassification leads to unnecessary avoidance of beta-lactams, which increases use of broader-spectrum agents and drives antimicrobial resistance. This is not just personal-it's epidemiological.
Leslie Douglas-Churchwell
November 19, 2025 AT 09:46Let’s be real-Big Pharma doesn’t want you to know you can outgrow penicillin allergies. 🤫 They make billions off the 'allergy label' because you’re stuck with expensive, toxic alternatives like vancomycin or clindamycin. And guess who pays? YOU. The healthcare system. Your insurance premiums. Your future kids who inherit your mislabeled record. They’ve been gaslighting us for decades. Get tested. Demand a referral. Don’t let corporate greed write your medical history. 🧬💉 #DrugAllergyTruth
shubham seth
November 20, 2025 AT 07:47Man, I saw this one guy in Mumbai who took a single dose of ibuprofen and his face swelled up like a balloon. He was fine after epinephrine, but now he’s terrified of every pill. Meanwhile, his cousin took the same thing for 10 years and never blinked. It’s not the drug-it’s your immune system playing Russian roulette. One shot, you’re dead. Next time, you’re fine. No logic. Just chaos. And doctors? They don’t even test. They just slap 'allergy' on the chart and move on.
saurabh lamba
November 21, 2025 AT 15:37So... we're just supposed to panic every time we get a rash? 😅 Like, what if I just got a sunburn and took Advil? Or ate something spicy? Life's too short to be scared of medicine. I mean, if I feel weird, I stop the pill. If I'm not choking, I'm probably fine. Chill out. The world's not out to kill you with penicillin.
Kiran Mandavkar
November 23, 2025 AT 09:53You people treat drug allergies like a meme. 'Oh, I'm allergic to aspirin.' No, you're not. You got a stomachache once. You’re not a martyr-you’re a liability. Every unverified allergy label you carry increases hospital costs, prolongs recovery, and endangers others by forcing doctors to use inferior, broad-spectrum antibiotics. You think you’re being careful? You’re being reckless. Get tested. Or shut up.
Eric Healy
November 24, 2025 AT 00:31Penicillin allergy testing is a joke. I got tested and they poked me with a needle and said 'nope you good' then gave me a pill and I broke out in hives 2 hours later. So now I'm allergic again? What even is this system? I'm just gonna stop taking meds unless I'm dying. That's my strategy. 😎
Holli Yancey
November 25, 2025 AT 10:17I just wanted to say thank you for writing this. My sister had DRESS syndrome after taking carbamazepine. She was in the ICU for 3 weeks. We didn’t know what was happening until a resident noticed the lymph nodes and fever. It’s terrifying. I wish more people knew how to spot the delayed signs. I’m sharing this with my family.
Gordon Mcdonough
November 26, 2025 AT 01:35Why are we letting the government and Big Pharma control what we can take? I’m not getting tested. I’m not letting some doctor tell me what my body can handle. If I feel bad after a pill, I stop it. That’s my right. And if I die? At least I died free. 🇺🇸
Jessica Healey
November 27, 2025 AT 22:43My mom’s allergic to sulfa. She had a reaction in 2005. She’s 70 now. She still won’t take any antibiotic that sounds even remotely like sulfa. I told her to get tested. She said, 'If it ain’t broke, don’t fix it.' But I know she’s missing out on better meds. I’m gonna take her to an allergist next month. Even if she hates it.