QT Prolongation Risk Calculator
Risk Assessment Tool
Enter your health factors to determine your risk of QT prolongation and related complications.
Your Information
Medications
Health Factors
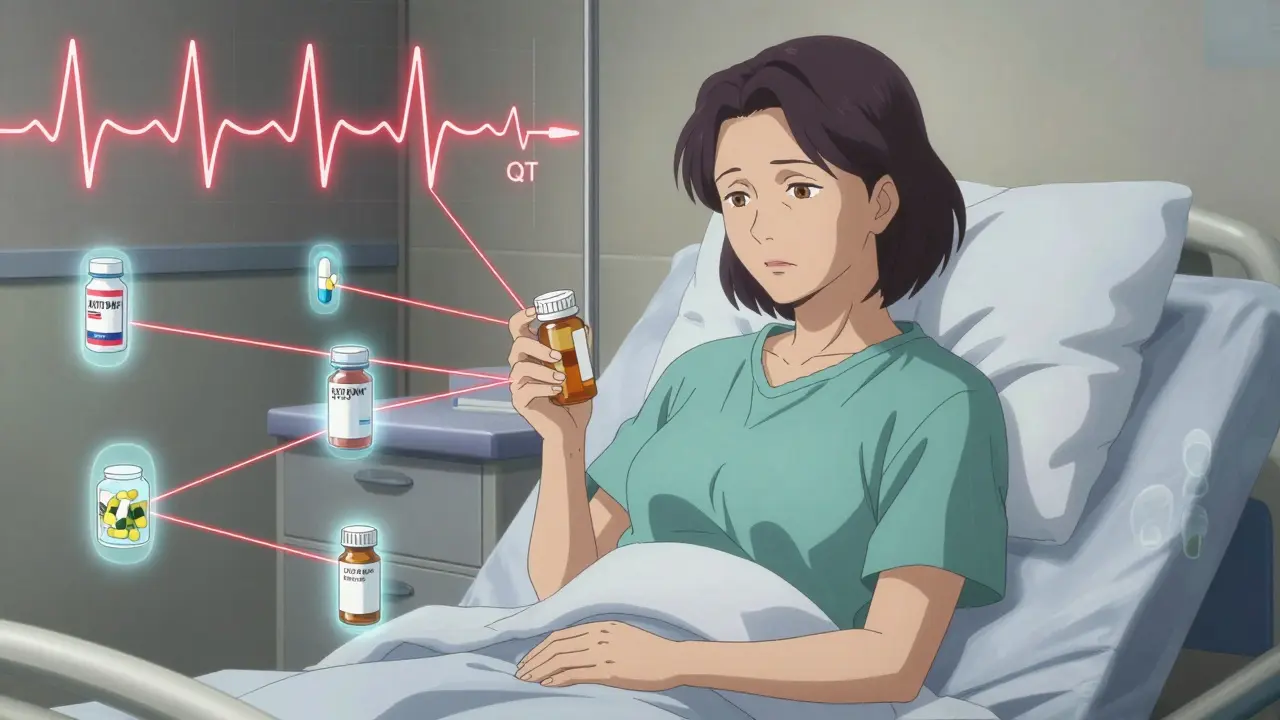
When a medication changes your heart’s rhythm in ways you can’t feel, it can kill you before you even know something’s wrong. That’s the silent danger of QT prolongation - a hidden electrical glitch in the heart that turns common prescriptions into potential killers. It’s not rare. It’s not theoretical. It’s happening right now in hospitals, clinics, and living rooms across the country.
What Exactly Is QT Prolongation?
The QT interval on an ECG measures how long it takes your heart’s lower chambers to recharge between beats. When that interval stretches too long - beyond 450 milliseconds in men or 470 in women - it creates a dangerous window for a chaotic rhythm called Torsades de Pointes. This isn’t just an ECG quirk. It’s a direct path to sudden cardiac death. The first major red flag came in the late 1990s when two popular antihistamines, terfenadine and astemizole, were pulled off shelves after dozens of deaths linked to QT prolongation. Since then, over 100 medications have been flagged for the same risk.Which Medications Are the Biggest Culprits?
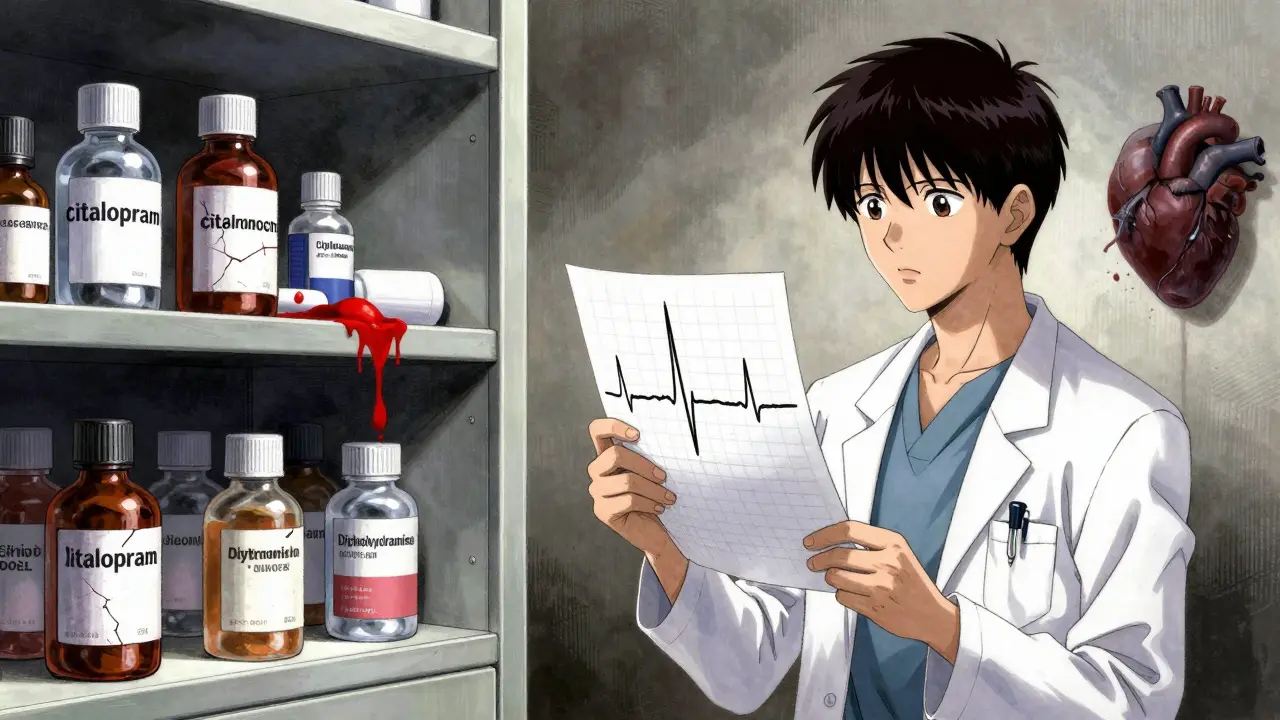
Not all QT-prolonging drugs are created equal. Some are high-risk by design, others are accidental offenders. Here’s where the real danger lies:- Class III antiarrhythmics like dofetilide and sotalol - these are meant to fix heart rhythms, but they can also trigger them. Dofetilide alone causes Torsades in about 3.3% of patients at standard doses.
- Antibiotics - moxifloxacin is the worst offender among common ones, extending QTc by 6-15 milliseconds. Erythromycin? It doubles your risk of sudden death. And if you’re taking it with a CYP3A4 inhibitor like ketoconazole or grapefruit juice? Risk jumps fivefold.
- Antidepressants - citalopram at 40mg daily can stretch QTc by 8.5 milliseconds. Escitalopram? Only 4.2. That’s a big difference. Yet many doctors still prescribe the higher dose without checking.
- Antipsychotics - drugs like haloperidol and ziprasidone carry serious QT risks, especially when combined with other meds or in patients with heart disease.
What makes this worse? Many of these drugs are prescribed for conditions that already strain the heart - depression, psychosis, chronic infection. You’re treating one problem while accidentally setting up another.
Who’s Most at Risk?
It’s not just about the drug. It’s about the person taking it. Three things turn a moderate risk into a life-threatening one:- Female gender - women are 2 to 3 times more likely to develop Torsades than men, even at the same drug dose and QTc level.
- Low potassium or magnesium - hypokalemia (potassium below 4.0 mEq/L) increases QT prolongation risk by 62%. A simple blood test can catch this before it’s too late.
- Structural heart disease - if you have heart failure, a prior heart attack, or enlarged heart, your risk of drug-induced arrhythmia spikes 10 to 100 times. The American Heart Association calls this the biggest modifier of risk.
And then there’s age. People over 65 take an average of 7.8 medications. About one in three of them is on a drug that can prolong QT. Polypharmacy isn’t just messy - it’s deadly when these interactions pile up.
Why Do Some People Have No Warning Signs?
This is the most terrifying part: 78% of people who died from QT-related arrhythmias had no prior signs of heart rhythm problems. Autopsies showed no structural damage. No history of fainting. No family history of sudden death. They were just taking their usual meds - a painkiller here, an antibiotic there, an antidepressant for depression - and their hearts suddenly stopped.Dr. Dan M. Roden from Vanderbilt put it bluntly: the link between QT prolongation and sudden death is more complex than we thought. For many, the real killer isn’t the arrhythmia itself - it’s the underlying illness, the electrolyte imbalance, or the drug interaction. The QT interval is just a signal, not the cause.
What’s Being Done to Stop This?
The FDA, NIH, and drug companies launched the CiPA initiative in 2013 to fix how we test new drugs for QT risk. Instead of just checking if a drug blocks one ion channel (hERG), they now look at how it affects the whole heart’s electrical system. This new method is 40% more accurate.Some hospitals are ahead of the curve. Mayo Clinic rolled out an automated ECG alert system in 2015 that flags high-risk QTc values and stops prescriptions before they’re filled. Result? A 37% drop in dangerous drug exposures.
Now, AI is stepping in. Verily Life Sciences’ QTguard system uses machine learning to analyze ECG patterns and cut false alarms by over half. That’s huge - because right now, 78% of QT alerts in hospitals are wrong. Doctors are tired of crying wolf. They start ignoring them.
What Should You Do - As a Patient or Provider?
You don’t need to panic. But you do need to act.For patients:
- Know your meds. If you’re on an antibiotic, antidepressant, or antipsychotic, ask: “Could this affect my heart rhythm?”
- Get a baseline ECG if you’re over 60, on multiple meds, or have heart disease.
- Don’t ignore dizziness or palpitations. They’re not just “side effects.” They could be your heart’s last warning.
For clinicians:
- Check potassium and magnesium before prescribing high-risk drugs.
- Use tools like AZCERT.org to see which drugs are risky and how they interact.
- Avoid combining QT-prolonging drugs. Even two low-risk ones can add up.
- Don’t order ECGs for every patient on low-risk meds like ondansetron. It creates alert fatigue and wastes resources.
The University of Michigan’s QT Clinician Toolkit says this: correcting low potassium cuts risk by 62%. Avoiding CYP3A4 inhibitors cuts it by 78%. That’s not magic. That’s medicine.
The Bigger Picture
QT prolongation isn’t just a drug safety issue. It’s a system failure. We’ve focused so much on measuring the QT interval that we’ve forgotten the person behind the ECG. We’ve scared patients off effective antidepressants because their QTc was 480 - even though their risk of death was lower than their risk of suicide without treatment.The European Heart Rhythm Association warns that 15-20% of heart failure patients have had life-saving meds stopped just because of a borderline QTc. That’s not protection. That’s harm.
The future? Personalized risk. The NIH’s All of Us program is collecting genetic data from a million people to find who’s naturally more vulnerable. Maybe your DNA tells you you’re at higher risk - and then we can tailor your meds accordingly.
Until then, the best defense is simple: know your meds. Know your numbers. Know your body. And don’t let a routine prescription become a silent killer.
Can a normal QTc still mean I’m at risk for sudden cardiac death?
Yes. QTc is just one piece of the puzzle. Someone with a normal QTc can still be at risk if they have low potassium, heart disease, or are taking multiple QT-prolonging drugs. The T-wave shape - especially the time from T-wave start to peak - is now considered a stronger predictor than QTc alone. In the ARIC study, each standard deviation increase in T-wave duration raised sudden death risk by 21%.
Is it safe to take citalopram if my QTc is 460?
Citalopram at 40mg/day is linked to QTc prolongation, and guidelines recommend not exceeding 20mg/day in adults, especially if QTc is above 450. At 460, you’re already in the prolonged range. Switching to escitalopram - which has less effect on QT - or lowering the dose to 20mg is safer. Always check potassium levels first. If they’re low, correct them before continuing.
Why do some drugs prolong QT more in women?
Women naturally have longer QT intervals than men due to hormonal differences, especially estrogen’s effect on heart ion channels. They also metabolize certain drugs slower, leading to higher blood levels. This combination makes them more sensitive to QT-prolonging effects. That’s why the threshold for concern is higher in women - 470ms versus 450ms in men.
Can I avoid QT risk by just avoiding antibiotics?
No. While antibiotics like moxifloxacin and erythromycin are risky, they’re not the only concern. Antidepressants, antipsychotics, anti-nausea drugs, and even some heart medications carry the same risk. The biggest danger comes from combinations - like taking an antibiotic with an antidepressant and a diuretic. It’s the mix, not just one drug.
Should I get an ECG before every new prescription?
Not for every drug. But yes - if you’re over 65, taking three or more medications, have heart disease, or are starting a high-risk drug like an antipsychotic or certain antidepressants. A single baseline ECG can save your life. Don’t wait for symptoms. Most people don’t feel anything until it’s too late.
Are over-the-counter meds a risk too?
Yes. Some antihistamines like diphenhydramine (Benadryl) can prolong QT, especially in high doses or when combined with other drugs. Herbal supplements like licorice root can lower potassium. Even certain cough syrups contain ingredients that interact dangerously. Always tell your doctor everything you’re taking - including what you buy at the store.
What Comes Next?
The tools are getting better - AI, genetic screening, smarter alerts. But the biggest gap isn’t technology. It’s awareness. Too many patients are told their QTc is “a little high” and told to “just watch it.” Too many doctors don’t check electrolytes. Too many pharmacies don’t flag dangerous combinations.The next time you’re prescribed a new medication, ask: “Could this affect my heart?” If the answer isn’t clear, ask for an ECG. Ask for a potassium check. Ask if there’s a safer alternative. You don’t need to be an expert. You just need to be informed.
Sudden cardiac death doesn’t come with a warning siren. But sometimes, it leaves behind a quiet line on an ECG - and a prescription bottle on the nightstand. Don’t ignore it.




Dee Humprey
January 3, 2026 AT 19:38One less thing to panic about tomorrow.
John Wilmerding
January 5, 2026 AT 03:44Peyton Feuer
January 5, 2026 AT 04:17Siobhan Goggin
January 7, 2026 AT 01:29Jay Tejada
January 7, 2026 AT 20:02Shanna Sung
January 8, 2026 AT 14:07Allen Ye
January 10, 2026 AT 00:14josh plum
January 11, 2026 AT 13:15