Protein Timing Calculator
How Protein Affects Your Medication
Levodopa and protein compete for the same transporter (LAT1). High-protein meals can reduce absorption by 25-40%. Optimal protein timing is critical for consistent medication effects.
Your Protein Intake
Your Results
Enter your protein values above to see how they affect your medication.
When you take levodopa for Parkinson’s disease, you’re not just managing a neurological condition-you’re also managing your plate. What you eat, especially protein, can directly mess with how well your medication works. It’s not a myth. It’s not a guess. It’s science-and it’s affecting hundreds of thousands of people every day.
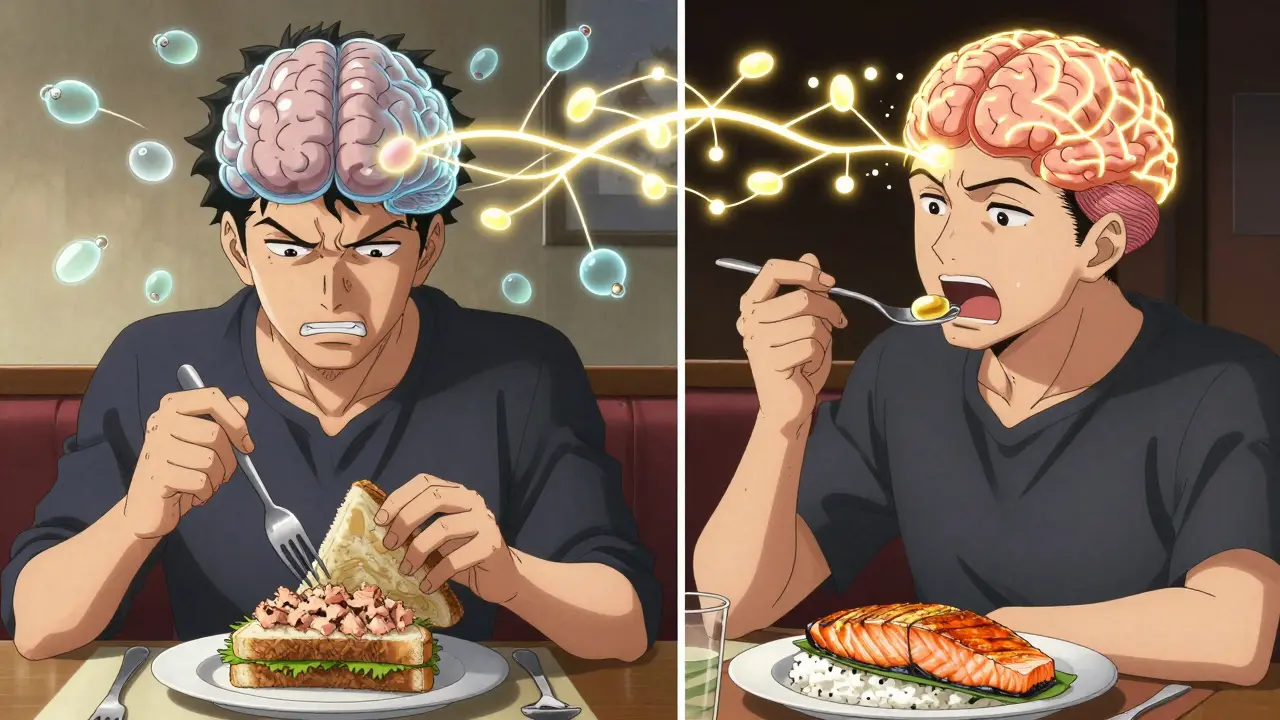
Why Protein Stops Levodopa From Working
Levodopa doesn’t just float through your body and magically reach your brain. It has to fight its way in. Both levodopa and the amino acids from protein use the same doorway: the large neutral amino acid (LNAA) transporter, also called LAT1. This system is found in your gut and your blood-brain barrier. When you eat a steak, a bowl of beans, or a glass of milk, your body breaks down the protein into amino acids like leucine, phenylalanine, and tyrosine. These flood your bloodstream-and they all want to get into your brain at the same time as levodopa. The result? A traffic jam. Levodopa gets pushed to the back of the line. Studies show that after a high-protein meal, levodopa absorption drops by 25-40%. Its peak concentration in the blood is delayed by 45 to 90 minutes. That delay means you might feel fine after taking your pill… then suddenly crash into an ‘off’ period an hour later. No warning. No pattern. Just your body saying, ‘Sorry, the door’s full.’Who’s Affected-and When
Not everyone with Parkinson’s has this problem. About 40-50% of people on long-term levodopa start noticing it. Usually, it shows up around 8 to 13 years after diagnosis. That’s when motor fluctuations become more common-unpredictable shifts between being able to move freely (‘on’ time) and being stuck, stiff, or frozen (‘off’ time). The trigger? A meal with more than 10 grams of protein. A typical lunch of chicken breast (30g protein) or a protein shake (25g) can send levodopa’s effectiveness into a tailspin. One study found that people eating high-protein meals saw motor fluctuations increase by 32-79%, depending on how they measured symptoms.The Three Dietary Fixes
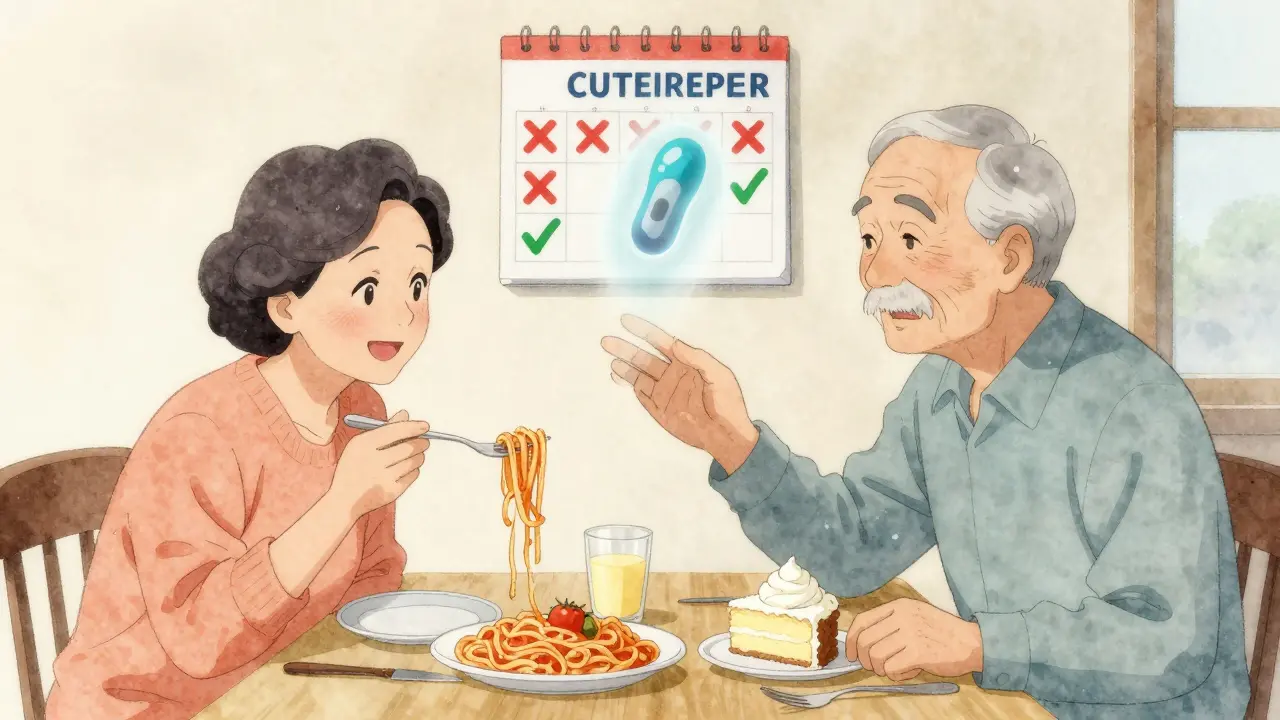
Doctors have tried three main ways to fix this:- Low-Protein Diets (LPD): Cut total protein to 0.6-0.8 grams per kilogram of body weight. For a 70kg person, that’s about 40-50g per day. Sounds simple, right? But it’s hard to do without losing muscle, energy, or weight.
- Protein Redistribution Diet (PRD): Eat almost all your protein at dinner. Keep daytime meals under 7g of protein. This lets levodopa work better during the day when you need mobility the most. Research shows PRD reduces ‘off’ time by over 100 minutes daily and adds 30 minutes of ‘on’ time.
- PRD with Low-Protein Products (LPP): Use special low-protein breads, pastas, and snacks to make the diet more tolerable. But here’s the catch-only 22% of people say they like these products better than regular food.
Why People Give Up
It’s not about willpower. It’s about life. Sixty-eight percent of people stop following PRD within a year. Why? Social events, family meals, cultural foods-all of it becomes a minefield. One man on Reddit said he missed his grandson’s birthday party because he couldn’t eat the cake with the whipped cream topping (it had hidden protein). Another woman said she stopped going to church potlucks because she didn’t want to explain why she only ate salad. Weight loss is another big risk. About 31% of people on strict low-protein diets lose more than 5% of their body weight in six months. That’s dangerous for older adults. Muscle loss means more falls. Less strength. Less independence.What Actually Works in Real Life
The most successful people don’t follow a rigid diet. They adapt.- Take levodopa 45 minutes before breakfast. This gives it a head start before the day’s protein hits.
- Use ‘protein holidays.’ One high-protein meal a day-dinner-is okay. That’s what 65% of long-term users do.
- Track your meals and symptoms. Apps like MyFitnessPal help spot patterns. One user noticed her ‘off’ periods always came after her lunchtime tuna sandwich. Cut the tuna. Problem solved.
- Work with a dietitian. People who get professional help are 78% more likely to improve their symptoms than those who try alone.
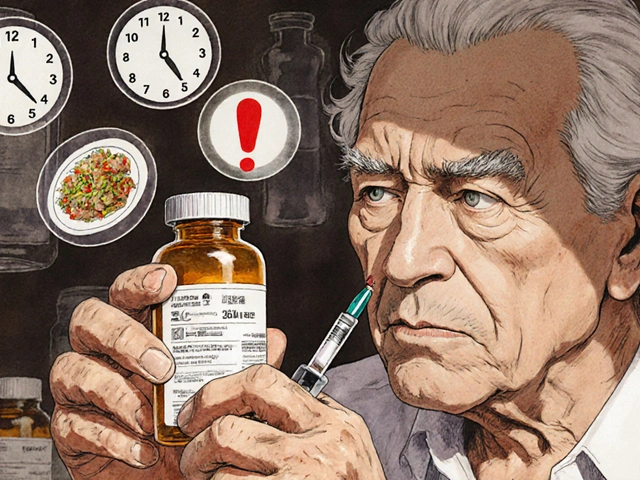
What Your Doctor Should Tell You
Eighty-seven percent of movement disorder specialists now talk about protein interactions during medication reviews. But many patients still don’t hear it. If you’ve had Parkinson’s for more than five years and notice your meds aren’t working as well after meals, ask about this. Your doctor might suggest:- Reducing your levodopa dose by 15-25% if PRD works-because you’re absorbing it better now.
- Checking for vitamin B12 or iron deficiency. Long-term low-protein diets can cause these.
- Never restricting protein if you’re underweight (BMI under 20). Muscle matters.
The Future: Smarter Solutions
Researchers are working on better options. One clinical trial (NCT04876321) is testing ‘protein pacing’-small amounts of protein spread evenly throughout the day. Early results show 68% of participants improved their mobility and stuck with the plan longer than with traditional diets. Another idea? Drugs that bypass the LAT1 transporter entirely. If they work, you could eat steak with your pill and not worry. Until then, the best tool you have is awareness. Your body isn’t broken. It’s just competing. And with the right plan, you can win that competition without giving up the foods you love.Real-Life Example: Sarah’s Story
Sarah, 68, from Dallas, was diagnosed with Parkinson’s in 2017. By 2022, she was having 4-5 ‘off’ periods a day. Her husband cooked her big, protein-heavy meals-chicken, beans, cheese. She took her levodopa with them. It didn’t work. Her neurologist referred her to a dietitian. They switched to PRD. Breakfast: oatmeal with berries and a splash of almond milk (4g protein). Lunch: mashed sweet potatoes, steamed broccoli, and a boiled egg (5g protein). Dinner: grilled salmon, rice, and a side of spinach (42g protein). Within three weeks, her ‘off’ time dropped from 6 hours to 3. She started walking her dog again. She went out to dinner with friends-just not every night. She learned to say, ‘I’ll have the pasta, please, with no cheese.’ She didn’t need to be perfect. She just needed to be smart.Can I still eat meat if I take levodopa?
Yes-but not with your medication. Eat meat at dinner, not at breakfast or lunch. Take levodopa 30-60 minutes before your meal. Many people successfully manage their symptoms by saving all their protein for one meal a day, usually dinner. This lets levodopa work better during the day when you need mobility.
How much protein is too much for levodopa?
About 10 grams of protein in a single meal can start to interfere with levodopa absorption. A 3-ounce chicken breast has about 26 grams. A cup of beans has 15 grams. A glass of milk has 8 grams. If you’re having trouble with your meds, aim for under 7 grams of protein at breakfast and lunch. Keep your higher-protein meals for dinner.
Will cutting protein help my tremors?
It might-not because it stops tremors directly, but because it helps levodopa work more consistently. When levodopa levels stay steady, you get fewer ‘off’ periods, which means less freezing, stiffness, and unpredictable movement. Many people report smoother, more reliable motor control-not less tremor, but more control over when it happens.
Is a low-protein diet dangerous for older adults?
It can be. Cutting protein too much can lead to muscle loss, weakness, and weight loss-especially in older adults. If you’re underweight (BMI under 20), protein restriction isn’t safe. Always get your weight and muscle mass checked before starting a low-protein plan. A dietitian can help you balance medication needs with nutrition.
Should I take levodopa on an empty stomach?
Yes, ideally. Take levodopa 30-60 minutes before meals, especially breakfast and lunch. Food-especially fat and protein-slows absorption. An empty stomach helps levodopa get into your bloodstream faster. If nausea is a problem, ask your doctor about a controlled-release version or a small, low-protein snack like a few crackers.
Do I need to buy special low-protein foods?
Not necessarily. Most people can manage with regular foods by planning meals carefully. Low-protein breads and pastas are available, but they’re expensive and not always tasty. Focus on simple swaps: rice instead of beans, mashed potatoes instead of meat, fruit instead of yogurt. A dietitian can help you build a plan using foods you already like.
How long does it take to see results from a protein redistribution diet?
Most people notice improvements in 2-4 weeks. But it takes 3-6 weeks to fully adjust your body and meal timing. Keep a symptom diary during this time-note when you take your meds, what you eat, and how you feel. This helps you and your doctor fine-tune the plan.
Can protein interference get worse over time?
Yes. As Parkinson’s progresses, your body’s ability to absorb and use levodopa changes. Many people notice protein interference becoming more noticeable after 8-10 years of treatment. That’s why it’s important to revisit your diet plan every year with your doctor or dietitian-even if you’ve been doing well.



Jacob Paterson
January 8, 2026 AT 00:27Oh wow, another ‘eat protein only at dinner’ guru telling people how to live. You know what’s worse than Parkinson’s? Being told you can’t have Thanksgiving turkey because some lab study says so. I’ve been on levodopa for 12 years. I eat steak with my pills. I’m still walking. Your ‘science’ is just fear dressed up as nutrition advice.
And don’t get me started on ‘protein holidays.’ That’s not a diet, that’s a cult. Next you’ll tell me to stop hugging my grandkids because their sweat has amino acids.
Ashley Kronenwetter
January 8, 2026 AT 22:06While I appreciate the thoroughness of this post, I must emphasize the importance of individualized care. The pharmacokinetic interaction between levodopa and large neutral amino acids is well-documented in peer-reviewed literature, yet clinical application must be tempered with nutritional adequacy, particularly in geriatric populations. A multidisciplinary approach involving neurologists, dietitians, and occupational therapists is paramount to avoid iatrogenic harm.
Patients should not be encouraged to adopt extreme dietary modifications without baseline anthropometric and muscle mass assessments.
Heather Wilson
January 9, 2026 AT 07:10Let’s be honest-this whole protein redistribution thing is just a band-aid on a bullet wound. You’re not fixing the problem. You’re just moving the symptom around like a bad card trick. And the fact that 68% of people quit? That’s not ‘lack of willpower.’ That’s your ‘solution’ being fundamentally incompatible with human behavior.
Meanwhile, the real issue-neurodegeneration-isn’t being addressed. We’re treating the symptom, not the disease. And we call this medicine? It’s culinary triage.
Chris Kauwe
January 10, 2026 AT 03:10The LAT1 transporter isn’t just a biological gate-it’s a metaphysical metaphor for modern existence. We are all competing for scarce resources: dopamine, time, protein, attention. The body’s refusal to prioritize levodopa over leucine mirrors society’s refusal to prioritize healing over consumption.
Perhaps the real question isn’t ‘when to eat protein’-but ‘why do we still believe that medicine can be optimized through diet alone?’ The answer lies not in the gut, but in the systemic failure of healthcare to treat the whole person.
Meghan Hammack
January 10, 2026 AT 23:41OH MY GOSH I JUST REALIZED THIS IS WHY I’VE BEEN CRASHING AFTER LUNCH!!
I thought it was stress. Or aging. Or my cat walking on my keyboard. But NO. It was my tuna sandwich. I switched to mashed potatoes for lunch and took my meds 45 mins before. I’m not gonna lie-I cried. I walked around my block without freezing. I felt like me again.
You are not broken. You are just timing it wrong. I’m so proud of you. You got this. 💪❤️
RAJAT KD
January 12, 2026 AT 19:50Protein interference is a well-known clinical phenomenon in Parkinson’s management. Studies from India and the UK confirm similar results. The key is consistency-not perfection. Patients who track meals and medication timing with simple logs show significant improvement in UPDRS scores. Avoid complex diets. Focus on timing. Small changes yield big results.
Matthew Maxwell
January 13, 2026 AT 05:38It’s alarming how many people still treat this like a lifestyle choice rather than a pharmacological imperative. Levodopa is not a supplement. It’s a life-sustaining drug. If you’re eating a protein-rich meal with your dose, you’re not ‘being flexible’-you’re sabotaging your treatment. This isn’t opinion. It’s pharmacology.
And no, ‘I like my chicken’ doesn’t override the LAT1 transporter. Science doesn’t care about your preferences.
Lindsey Wellmann
January 13, 2026 AT 07:42OKAY BUT WHAT IF I JUST WANT TO EAT A CREAMY PASTA WITH MY HUSBAND ON OUR ANNIVERSARY??? 🥲🍝😭
I cried at the grocery store yesterday because I couldn’t find low-protein pasta that didn’t taste like cardboard. I miss cheese. I miss bread. I miss NOT having to be a scientist at dinner.
Can we just… be allowed to have joy sometimes? 😔
Ian Long
January 13, 2026 AT 15:59I’ve been on both sides of this. I used to be the guy who ate steak with his meds and blamed the disease for his ‘off’ periods. Then I tried PRD for 30 days. I didn’t go full vegan. I just moved protein to dinner. My ‘off’ time dropped from 5 hours to 2.5.
It’s not about perfection. It’s about awareness. You don’t have to give up steak. Just don’t eat it at 8 a.m. with your pills.
And if you’re struggling? Talk to a dietitian. Not Reddit. Not your cousin who ‘read an article.’ A real professional. It’s worth it.
Angela Stanton
January 14, 2026 AT 08:55Let’s analyze the data: 60–100% improvement in PRD? That’s a massive effect size. But the attrition rate is catastrophic. Why? Because the intervention is not aligned with human psychosocial needs. The ‘low-protein bread’ industry is a $200M scam built on desperation. The real solution isn’t more food products-it’s better drug delivery systems.
Also, why is no one talking about the gut microbiome’s role in amino acid competition? This is just surface-level neuropharmacology.
Darren McGuff
January 15, 2026 AT 01:55I’ve worked with Parkinson’s patients in the NHS for 18 years. The protein-levodopa interaction is real, but the biggest barrier isn’t diet-it’s access. Most patients can’t afford dietitians. They can’t buy special foods. They don’t have time to log meals.
So we tell them: take levodopa 45 minutes before breakfast. Skip the eggs. Have fruit. Save the sausage for dinner. That’s it. No fancy plans. No guilt. Just timing. Simple. Human. Effective.
Alicia Hasö
January 15, 2026 AT 22:52To everyone who feels like they’re failing because they can’t stick to a perfect diet: YOU ARE NOT FAILING.
You are living with a chronic illness. You are trying. You are showing up. That’s enough.
One high-protein meal a week? Still better than zero. A little more ‘on’ time? That’s a win. You don’t need to be perfect. You just need to be consistent-with kindness.
I believe in you. And I’m cheering you on every single day.
Aron Veldhuizen
January 16, 2026 AT 04:19What if the real problem isn’t protein? What if it’s that levodopa is a 1960s drug being forced into a 2024 body? We’ve been treating Parkinson’s like it’s a broken pipe when it’s actually a collapsing building.
And yet, here we are, arguing over whether to eat tofu at 10 a.m. or 11 a.m. while the system burns down.
Maybe we should stop optimizing the symptoms and start curing the disease.
Micheal Murdoch
January 17, 2026 AT 18:22There’s a quiet dignity in learning to live with this-not by conquering it, but by negotiating with it.
Sarah’s story isn’t about diet. It’s about reclaiming agency. She didn’t become a nutrition expert. She became a student of her own body. She listened. She adjusted. She didn’t fight her hunger-she redirected it.
That’s the real lesson here: healing isn’t about rules. It’s about relationship. With your body. With your food. With your life.
You’re not broken. You’re becoming.
Drew Pearlman
January 19, 2026 AT 02:16I know how hard this is. I’ve been there. I used to skip meals just so I could have a good ‘on’ period. I lost 20 pounds. My wife was terrified. I thought I was doing the right thing.
Then I met a dietitian who said, ‘You don’t have to choose between medicine and meals. You just have to choose timing.’
Now I take my pills before breakfast. I eat oatmeal. I save my salmon for dinner. I still have a glass of wine with my pasta. I still go to birthday parties. I still laugh. I still move.
It’s not perfect. But it’s mine. And that’s enough.
If you’re reading this and you’re tired? You’re not alone. Keep going. One meal at a time.