Shingles isn’t just a rash. It’s a sharp, burning, sometimes electric pain that can last for weeks-or even years-if not treated right. If you’ve ever felt that kind of pain on one side of your body, you know it doesn’t go away with a bandage or ibuprofen. The good news? You can stop it from getting worse-if you act fast.
What Causes Shingles?
You didn’t catch shingles from someone else. It came from inside you. Years ago, you had chickenpox. The virus that caused it-varicella-zoster-never left. It hid in your nerve roots, quiet and dormant. Then, for reasons doctors still don’t fully understand, it woke up. Maybe your immune system got weak from stress, aging, or illness. Suddenly, the virus started copying itself along a nerve pathway, triggering a painful rash. This is shingles, or herpes zoster.
One in three Americans will get it in their lifetime. The risk jumps after 50. By 80, nearly half of people have had it. And if you’re over 60? Your chance of developing long-term nerve pain-called post-herpetic neuralgia-goes up to 30%.
Why Timing Matters More Than Anything
The single biggest thing that changes your outcome? How soon you start treatment.
Antiviral drugs like valacyclovir, acyclovir, and famciclovir don’t cure shingles. But they can slash your recovery time by days and cut your pain by up to 30%. That’s not a small win. It means less time off work, fewer sleepless nights, and a much lower chance of ending up with chronic pain.
But here’s the catch: these drugs only work if you start them within 72 hours of the first sign of the rash. That’s three days. Not five. Not a week. Three.
Studies show that people who begin treatment within 48 hours report 40-50% shorter illness duration. After 72 hours, the virus has already spread too far. The antivirals can still help, but their power drops sharply. Waiting? You’re gambling with your nerves.
The Three Antiviral Options
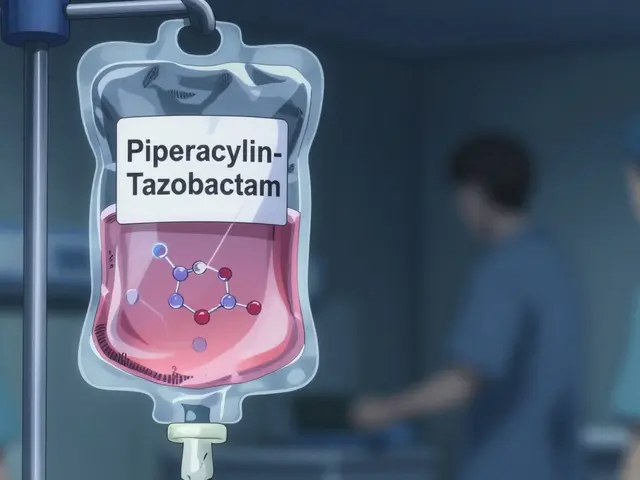
There are three FDA-approved antivirals for shingles. All work similarly, but their dosing and convenience differ.
- Valacyclovir (Valtrex): 1,000 mg three times a day for 7 days. Easier to take-fewer pills. Studies suggest it reduces pain slightly better than acyclovir.
- Acyclovir (Zovirax): 800 mg five times a day for 7-10 days. Cheaper, but you have to take it every 4-5 hours, including at night. Hard to stick with.
- Famciclovir (Famvir): 500 mg three times a day for 7 days. Similar dosing to valacyclovir. Slightly less data on pain reduction.
Most doctors now start patients on valacyclovir. It’s the most practical. You take it with food, and you’re done with three doses a day. Side effects? Headache (13%), nausea (9%), dizziness (7%). Most people tolerate it fine.
For people with weakened immune systems-those on chemo, steroids, or with HIV-doctors often give higher doses or longer courses. These patients are at higher risk for severe outbreaks, eye damage, or skin infections. Delaying treatment here can be dangerous.

What About Post-Herpetic Neuralgia?
This is the nightmare scenario: the rash clears, but the pain doesn’t. It’s not just soreness. It’s burning, stabbing, itching pain that lingers for months-or years. About 10-18% of shingles patients get it. Over 60? It’s 30%.
Here’s the confusing part: some studies say antivirals don’t prevent it. Others say they do. The Cochrane Review says acyclovir doesn’t reduce long-term pain. But a 2011 review in PubMed found early treatment lowered the risk of chronic pain by 30-40%.
Why the disagreement? It’s messy. Some patients start treatment too late. Others have other health problems. But real-world data tells a clearer story. On PatientsLikeMe, 62% of 1,200 people who took antivirals within 72 hours said they avoided long-term pain. That’s not perfect-but it’s better than nothing.
And here’s something new: long-term, low-dose valacyclovir (500 mg daily) may help prevent recurring eye damage in people with shingles affecting the eye. The Zoster Eye Disease Study found it cut new flare-ups by 30% and reduced the need for nerve pain meds like gabapentin by 25%. For those with eye involvement, this is now a standard recommendation.
Pain Management: Beyond the Antiviral
Antivirals fight the virus. But they don’t fix the nerve damage. That’s where pain management comes in.
For mild pain, over-the-counter options like ibuprofen or acetaminophen help. But for moderate to severe pain? You need stronger tools.
- Gabapentin or pregabalin: These are anti-seizure drugs that calm overactive nerves. Start low-300 mg at night-and slowly increase. Side effects: drowsiness, dizziness, weight gain. But they work for nerve pain.
- Amitriptyline: An old-school antidepressant. Take 25-75 mg at night. It helps with sleep and pain. Don’t be scared of the word “antidepressant”-it’s not for depression here.
- Lidocaine patches: Stick these on the painful area for 12 hours on, 12 off. No pills. No system-wide side effects. Great for localized pain.
- Capsaicin cream (0.075%): Made from chili peppers. It burns at first, then numbs. Apply 3-4 times a day. Works best after the rash is gone.
Opioids? Only for severe, short-term pain. They don’t work well for nerve pain long-term and carry addiction risks. Doctors avoid them unless absolutely necessary.
Some clinics now use a combination: antiviral + gabapentin + lidocaine patch from day one. This approach reduces hospital visits and speeds recovery.
The Vaccine: Your Best Shield
The best way to avoid shingles? Don’t get it.
The Shingrix vaccine is more than 90% effective at preventing shingles. Even if you get it after vaccination, the outbreak is usually milder. You need two shots, 2-6 months apart. It’s recommended for everyone 50 and older-even if you had shingles before or got the old Zostavax vaccine.
Shingrix doesn’t treat an active outbreak. But if you’re 50+, and you haven’t gotten it yet? Talk to your doctor. It’s one of the most effective vaccines you’ll ever get.

What to Do Right Now
If you feel tingling, burning, or pain on one side of your body-especially on your chest, face, or back-and you haven’t had a rash yet? Call your doctor today. Don’t wait for the rash to appear. Early symptoms can start 1-5 days before the rash.
Don’t assume it’s a pulled muscle. Don’t wait to see if it gets worse. If you’re over 50, and you have unexplained nerve pain in a band-like pattern? Shingles is likely.
Even if you’re younger, don’t ignore it. The sooner you start antivirals, the less pain you’ll have-and the less chance you’ll end up with long-term nerve damage.
Cost and Accessibility
A 7-day course of valacyclovir costs $85-$150 without insurance. With Medicare Part D or private insurance? Often under $20. Many pharmacies offer discount programs.
And here’s the kicker: early treatment saves money. A 2022 study found it cuts total healthcare costs by $487 per person by preventing ER visits, hospitalizations, and long-term pain meds.
It’s not just about pills. It’s about avoiding months of pain, lost work, and depression.
What’s Next in Research
Doctors are now studying whether combining antivirals with short-term steroids (like prednisone) helps reduce acute pain. Early results look promising-but the risk of suppressing your immune system means it’s still debated.
Researchers are also looking at genetic factors that make some people more prone to severe pain. One day, treatment might be personalized: your DNA tells your doctor which pain meds will work best for you.
For now, the rules are simple: act fast, treat early, and protect yourself with the vaccine.

Tony Du bled
December 21, 2025 AT 23:21Been there. Got the rash, the pain, the sleepless nights. Took valacyclovir at day two and it made all the difference. Didn't turn into a ghost of my former self. Don't wait. Seriously.
Kathryn Weymouth
December 22, 2025 AT 11:29The data on antivirals reducing post-herpetic neuralgia is indeed conflicting, but the real-world patient reports-like those from PatientsLikeMe-are compelling. Early intervention correlates strongly with better outcomes, even if RCTs are messy. The 30-40% reduction in chronic pain risk isn't negligible, especially for those over 60.
Julie Chavassieux
December 24, 2025 AT 02:32So basically if you're old you're just gonna get roasted by your own immune system? Cool. Glad I'm not you.
Herman Rousseau
December 25, 2025 AT 14:13Shingrix saved my life. Got it at 52. Two shots. No shingles. No pain. No drama. If you're 50+ and haven't gotten it yet, you're playing Russian roulette with your nerves. Do yourself a favor and call your doctor tomorrow. Seriously. Your future self will thank you.
Vikrant Sura
December 26, 2025 AT 10:55Why are we even talking about this? Just take ibuprofen and deal with it. Pharma wants you scared so they can sell you pills.
Candy Cotton
December 27, 2025 AT 22:03It is imperative that all citizens of this nation adhere to the highest standard of medical compliance. Failure to initiate antiviral therapy within seventy-two hours constitutes a dereliction of personal responsibility and a burden on the healthcare system.
Jeremy Hendriks
December 29, 2025 AT 09:37Shingles isn't a disease-it's a metaphor. The virus doesn't just wake up, it remembers. It remembers your late nights, your skipped meals, your unprocessed grief. It's not your immune system failing-it's your soul screaming for attention. And the antivirals? They're just bandaids on a wound that needs a reckoning. The real cure? Living differently. Before it's too late.
Gabriella da Silva Mendes
December 31, 2025 AT 09:26OMG I got shingles last year and it was THE WORST THING EVER 😭 I cried for three days straight and my cat left me. I took gabapentin and it made me feel like a zombie but at least I didn't die. Also I got Shingrix after and now I'm basically a superhero. 💪💉 #ShinglesSucks #VaccineWins
Kiranjit Kaur
January 1, 2026 AT 20:23My aunt in India got shingles and couldn't afford the meds. She used neem paste and turmeric. It didn't cure it, but she didn't get the nerve pain either. Maybe we need to look beyond big pharma for simple, affordable solutions too.
Sai Keerthan Reddy Proddatoori
January 2, 2026 AT 13:48They say it's from chickenpox but I think it's a government bioweapon. They put it in the water so old people get sick and die faster. Vaccines are just the next step. Don't trust the FDA. Don't trust the doctors. Trust yourself.
Sam Black
January 2, 2026 AT 14:20Back in '09, I had shingles on my neck. Took the antivirals, used lidocaine patches, and slept with a cold pack taped to my shoulder like a weirdo. Didn't get the long-term pain. The key? Treat it like a fire-smother it fast. And yeah, get the vaccine. It's not optional anymore. It's wisdom.