Telehealth Travel Time & Cost Calculator
How Telehealth Saves Rural Patients
Based on article data: Rural patients are 23% more likely to experience preventable adverse drug events. Telehealth reduces travel time and provides real-time side effect monitoring. Calculate your potential savings.
Enter round-trip distance to your nearest clinic
Current fuel cost in your area
Your car's fuel efficiency
Your hourly income value
For millions of people living in rural and remote areas, taking medication for chronic conditions like high blood pressure, depression, or blood clots isn’t just about sticking to a schedule-it’s about staying alive. But getting timely help when side effects show up? That’s a daily challenge. Traveling hours to a clinic isn’t always possible. Waiting weeks for an appointment can turn a mild reaction into a hospital emergency. That’s where telehealth comes in-not as a luxury, but as a lifeline.
Why Rural Patients Face Higher Risks
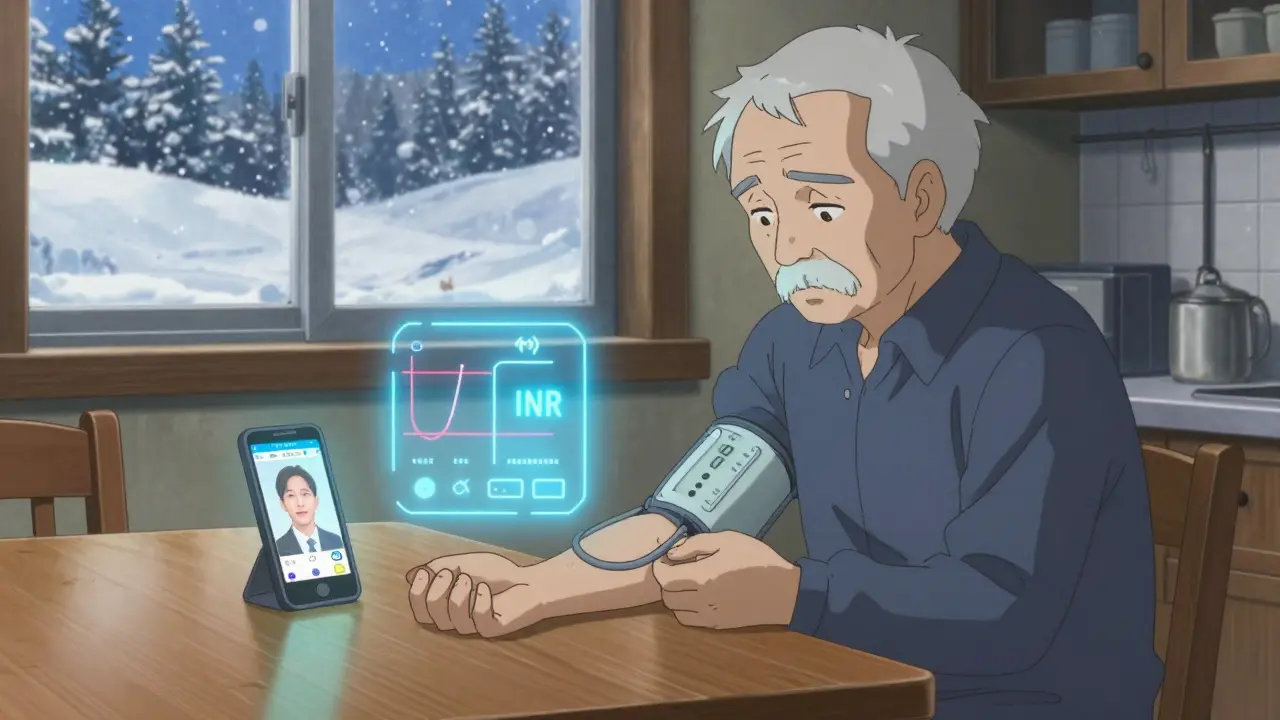
Rural patients are 23% more likely to experience preventable adverse drug events than those in cities, according to a 2020 Health Affairs analysis. Why? It’s not just distance. It’s the lack of nearby pharmacists, fewer specialists, and delayed access to emergency care. A patient on warfarin might notice their INR levels creeping up, but without a nearby lab or doctor, they wait until they’re dizzy or bruising easily. By then, it’s too late. Same with antidepressants-70% of rural patients report side effects like tremors, dizziness, or suicidal thoughts, but only 40% report them to their provider in time. Telehealth isn’t just convenient here; it’s a safety net.How Telehealth Monitors Side Effects in Real Time
Modern telehealth for side effect monitoring isn’t just a video call. It’s a system. Patients use FDA-cleared devices that sync automatically with their phones: Bluetooth blood pressure cuffs, smart pill dispensers that log when doses are taken, and wearable sensors that track heart rate and movement. One system used in Mississippi tracks INR levels at home-patients prick their finger once a week, and the device sends results directly to a pharmacist. If the number climbs too high, they get a call within an hour. No waiting. No driving. Video visits are part of it, but they’re not the whole story. Many programs now use asynchronous monitoring: patients text or upload symptoms through an app-"I feel shaky," "My legs are swollen," "I can’t sleep"-and the system flags it for review. AI tools like IBM Watson’s MedSafety can now predict which patients are at risk for severe reactions with 84% accuracy by analyzing patterns in symptoms, meds, and vitals. That means a patient might get a warning before they even realize something’s wrong.What Works Best in Practice
The most successful programs share three things: dedicated staff, integration with existing records, and simple tech. The University of Mississippi’s anticoagulation program keeps 92% of patients engaged by pairing home INR monitors with weekly video calls from a pharmacist-not a nurse, not a doctor, but a pharmacist trained in blood thinners. Why? Because pharmacists know the drugs inside out. They spot interactions, adjust doses, and explain side effects in plain language. These programs also connect directly to electronic health records like Epic or Cerner. That means if a patient reports nausea in the app, the doctor sees it alongside their latest lab results, not in a separate file. And the tech? It’s designed for people who aren’t tech-savvy. Apps use big buttons, voice prompts, and simple icons. Still, 68% of rural patients need at least two training sessions to use them well-and seniors need more than three.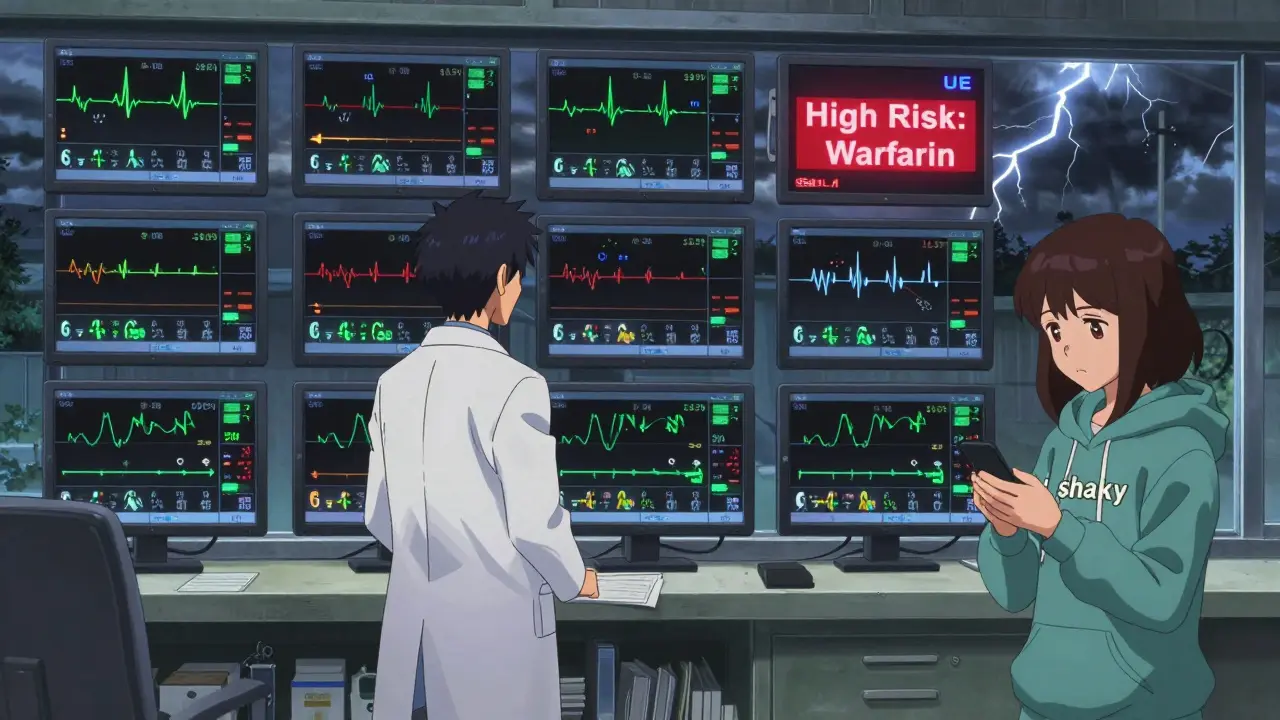
The Hidden Barriers
Not everyone can use it. About 28% of rural Americans don’t have broadband that meets federal standards. In some areas, the internet drops during storms. Cell service is spotty. Even when the tech works, 34% of seniors over 65 say they struggle with smartphones. And then there’s the human factor: 29% of patients feel telehealth is "impersonal." One woman in West Virginia said her provider couldn’t see her tremors because the video was blurry. That’s not just bad tech-it’s a missed diagnosis. Another problem? Follow-up. A 2022 study found 33% of rural telehealth programs don’t have clear protocols for what happens after a side effect is reported. Does the patient get a call? A visit? A referral? Without a system, even the best app fails.Who’s Getting Left Behind
Black rural patients are 1.8 times less likely to receive telehealth side effect monitoring than white patients, according to the AHRQ. Why? It’s not one thing. It’s a mix: fewer clinics in their areas, less trust in the system, language barriers, and lack of multilingual support. Only 87% of successful programs offer this. And reimbursement is uneven. Medicare pays $51 for 20 minutes of remote monitoring. But only 63% of private insurers match that. Rural clinics can’t afford to run programs if they’re not paid fairly. Even worse, when big urban telehealth companies expand into rural areas, they often take patients-and revenue-away from local clinics. One study found rural hospital income dropped 15% when patients switched to distant providers. That means fewer local staff, fewer resources, and eventually, fewer services for everyone.What’s Changing in 2026
The good news? Things are moving. In January 2024, CMS started paying up to $27 per day for asynchronous monitoring-no video needed. That’s huge for patients with bad internet. The FCC’s Rural Digital Opportunity Fund is spending $20.4 billion through 2025 to fix broadband. And more pharmacies are launching telehealth teams. Vanderbilt’s study showed a 43% drop in severe side effects when pharmacists led the monitoring. New tools are coming too. Wearable sensors in Arkansas can now detect subtle movement changes linked to antipsychotic side effects-like tardive dyskinesia-with 91% accuracy. That’s something a video call might miss. And AI is getting smarter, learning from thousands of rural patient reports to predict problems before they happen.


Jarrod Flesch
January 20, 2026 AT 17:19Love this breakdown. I’ve seen this play out in rural Australia-old folks on warfarin with no nearby pharmacy, just a phone and a dumbphone. The Bluetooth INR monitor saved my uncle’s life. No drama, no 3-hour drive, just a text: "Your INR’s high. Call your doc." Simple. Brilliant.
And yeah, the tech ain’t perfect-but it’s better than waiting for a stroke.
Rod Wheatley
January 21, 2026 AT 17:46YES! YES! YES!!!
Pharmacists are the unsung heroes of rural telehealth!!!
They know the drugs, the interactions, the side effects, the timing, the patient’s history-MORE than most docs in these areas!!!
And they’re trained to talk to people-not just order tests!!!
Why are we still letting doctors monopolize care when pharmacists are literally sitting there with the medication in their hands???
Let pharmacists lead. Let them adjust. Let them call. Let them save lives!!!
Also-voice prompts on apps? GENIUS. My grandma uses one now. She says it feels like talking to her pharmacist again.
Melanie Pearson
January 22, 2026 AT 13:40As a policy analyst with 18 years in public health, I must emphasize: this is not a technological failure-it is a systemic abandonment of rural populations. The 28% broadband gap? It’s not an accident. It’s intentional underinvestment. The reimbursement disparity? Deliberate. The lack of multilingual support? A failure of federal mandate enforcement.
And let’s not pretend AI is the savior-it’s a Band-Aid on a hemorrhage. Without equitable infrastructure, telehealth becomes a luxury for the digitally privileged, not a right for the medically vulnerable.
Stop glorifying apps. Start funding cell towers.
Uju Megafu
January 23, 2026 AT 08:13Oh my GOD, this is so obvious. Why are we even having this conversation? Of course rural people die more from side effects-they’re poor, they’re isolated, they’re ignored. And now we’re giving them a PHONE APP to fix it? LOL. Like if they just tried harder, they wouldn’t have a stroke.
Meanwhile, the same people who run these telehealth startups are flying to Aspen for retreats. They don’t live where the patients live. They don’t see the snowed-in roads or the dead cell towers.
It’s performative activism wrapped in a Bluetooth cuff. Sad.
Coral Bosley
January 24, 2026 AT 13:46I’ve been on antidepressants for 11 years. I’ve had tremors so bad I couldn’t hold a cup. I’ve had suicidal thoughts so loud I screamed into my pillow. I never told anyone. Not because I didn’t want to-but because I was terrified they’d lock me up. Or worse-stop my meds.
Then I got the app. It asked every day: "Are you safe?"
One day I typed: "No."
Two hours later, a pharmacist called. Not a robot. Not a script. A real person. She didn’t judge. She didn’t panic. She just said, "Let’s get you help."
I cried for an hour after.
That’s not tech. That’s humanity.
Ben McKibbin
January 25, 2026 AT 20:45This is one of the most balanced, data-rich, and human-centered pieces I’ve read on rural healthcare in years. The stats don’t lie: 23% higher preventable events? That’s a moral crisis.
But what’s truly remarkable is how the solution isn’t about fancy gadgets-it’s about trust, simplicity, and local ownership. A pharmacist who knows your name, your dog, your grandson’s birthday-that’s the real AI.
And yes, the tech must be dumb-proof. My 78-year-old aunt uses an app with one button. It says: "Call me if you feel weird." She presses it. Someone calls back. Done.
Let’s stop over-engineering. Start humanizing.
Alex Carletti Gouvea
January 26, 2026 AT 11:05Another liberal fantasy dressed up as healthcare. You want to fix rural medicine? Stop importing foreign apps and start supporting American clinics. Stop letting Silicon Valley CEOs profit off our grandparents’ suffering. Build real clinics. Pay real doctors. Train real nurses. Not some app that asks if you’re "safe."
And why is Medicare paying $27 a day for text messages? That’s a scam. We need boots on the ground-not bots on the phone.
Stop outsourcing our healthcare to tech bros.
Amber Lane
January 28, 2026 AT 01:54Yuri Hyuga
January 28, 2026 AT 12:34Let’s zoom out for a moment. This isn’t just about drugs or devices. It’s about dignity. It’s about the elderly woman in West Virginia who doesn’t want to drive 80 miles to be told, "It’s just anxiety." It’s about the Black man in Mississippi who fears his symptoms will be dismissed because of his skin tone. It’s about the fact that we’ve normalized neglect as policy.
Telehealth isn’t the answer-it’s the beginning of a reckoning. We have the tools. We have the data. What we lack is the collective will to treat every life as equally worthy of care.
So ask yourself: if this were your mother, would you accept a blurry video call as enough?
Because right now, millions are getting exactly that.
Barbara Mahone
January 29, 2026 AT 23:52As someone raised in rural Ohio, I can say this: the biggest barrier isn’t tech or money-it’s shame. Many patients won’t report side effects because they don’t want to be a burden. They think, "I’m fine. I’ll tough it out."
That’s why the daily check-ins matter. Not because they’re smart tech-but because they say: "You matter. We’re here. You’re not alone."
That’s the quiet revolution here. Not the Bluetooth cuff. The connection.
Kevin Narvaes
January 30, 2026 AT 21:55ok so like… telehealth is cool and all but like… why are we trusting algorithms to catch side effects? what if the AI misses something? what if the phone dies? what if the patient is just… tired of answering questions every day?
also why is everyone so obsessed with pharmacists? i mean, sure they know drugs, but can they tell if your face is swollen? can they see if you’re shaking? no. you need a doctor. a real one. with eyes.
also why is this article so long? i read half and got bored. just say what u mean.
Malvina Tomja
January 31, 2026 AT 06:00Let’s be real-this whole telehealth push is just a cover for cutting rural hospitals. Why pay for a clinic when you can send a text? Why hire a nurse when an app can ask, "How are you feeling?"
It’s not innovation. It’s cost-cutting with a pretty UI.
And don’t even get me started on the "AI predicts side effects" nonsense. If your algorithm is trained on urban data, it’ll miss everything that matters in the sticks.
Also, who wrote this? A PR rep for Teladoc? It’s all fluff and no accountability.
MARILYN ONEILL
February 1, 2026 AT 10:01Ugh. Another one of these "rural people are helpless" articles. Newsflash: they’re not helpless. They’re just lazy. If they wanted to use the app, they’d learn. If they wanted broadband, they’d move to a town with it. Stop coddling people who won’t take responsibility.
Also, why are we paying for this? Why not just tell them to go to the ER if they feel bad? That’s what I’d do. Stop making everything a crisis.
And stop saying "Black patients are less likely." That’s just race-baiting. They don’t use tech because they don’t care. End of story.
MAHENDRA MEGHWAL
February 1, 2026 AT 12:55As a healthcare worker from rural India, I recognize every challenge described here. Distance, lack of specialists, unreliable connectivity, distrust in systems-all familiar.
But I also know what works: community health workers. Trained locals who carry simple devices, visit homes, and translate tech into trust. No video calls needed. Just presence.
Telehealth must not replace human touch-it must empower it. The best systems blend tech with tradition. Not the other way around.
Kelly McRainey Moore
February 1, 2026 AT 16:13I work at a small clinic in rural Maine. We started with just warfarin patients and a $500 Bluetooth INR monitor. Now we’ve got 120 people on it. No one’s had a bleed in 18 months.
Our secret? We sit with them. First visit: we hold their hand while they set up the app. Second visit: we laugh when they spill coffee on the device. Third visit: they teach their neighbor.
It’s not magic. It’s just care.
And yes-we still do in-person checkups. The app just helps us see them sooner.