Arrhythmia Risk Checker
How This Tool Works
This tool helps you understand your risk of developing dangerous heart rhythm problems from medications. It checks your medications against known arrhythmia-causing drugs and factors in your age and electrolyte status to calculate your risk level. Remember, this is for informational purposes only, not medical advice.
Key Risk Factors
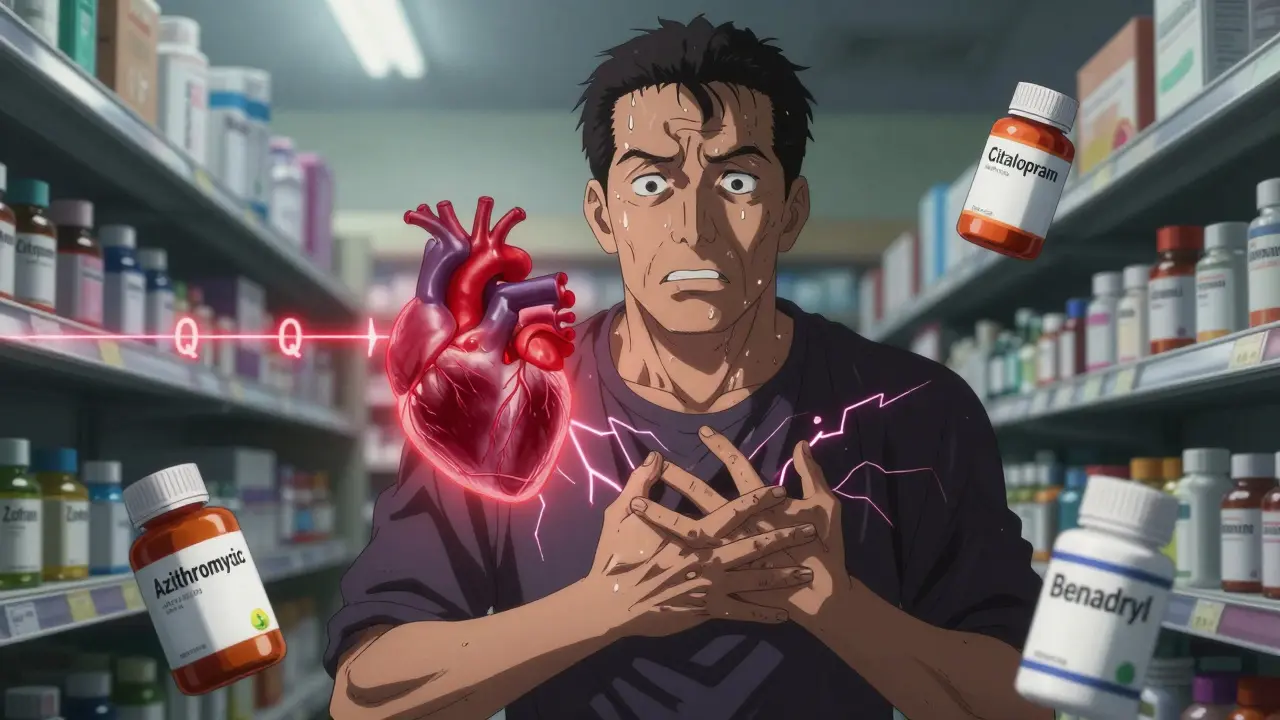
More than 400 common medications can trigger dangerous heart rhythm problems - and many people have no idea they’re at risk. It’s not just the old-school drugs like quinidine. Today, it’s antibiotics you pick up at the pharmacy, antidepressants your doctor prescribed, even over-the-counter cold meds. These aren’t rare side effects. They happen often enough to send 100,000 to 150,000 Americans to the hospital every year. And the worst part? Many of these cases are preventable.
What Exactly Is a Drug-Induced Arrhythmia?
A drug-induced arrhythmia is when a medication messes with your heart’s electrical system, causing it to beat too fast, too slow, or irregularly. The most common and dangerous type involves QT prolongation - a delay in the heart’s recovery phase after each beat. This tiny timing error can spiral into torsades de pointes, a life-threatening ventricular rhythm that can lead to sudden cardiac arrest.
It’s not just one mechanism. Some drugs block potassium channels. Others mess with sodium or calcium flow. Some trigger electrolyte imbalances. A few even cause thyroid dysfunction, like amiodarone, which ironically treats arrhythmias but can cause them too. Even medications you think are safe - like certain antihistamines or diabetes pills - can be culprits.
Which Medications Are Most Likely to Cause Problems?
Not all drugs carry the same risk. Here are the top offenders, broken down by category:
- Antibiotics: Macrolides like azithromycin and fluoroquinolones like levofloxacin. Risk spikes in the first week of use.
- Antidepressants and antipsychotics: Citalopram, escitalopram, haloperidol, and ziprasidone. These are among the most common causes in older adults.
- Antiarrhythmics themselves: Flecainide and propafenone can worsen atrial flutter. Amiodarone, despite being used to treat arrhythmias, causes atrial fibrillation in 2-5% of users.
- Diuretics: Furosemide and hydrochlorothiazide deplete potassium and magnesium - key minerals your heart needs to beat properly.
- Digoxin: Used for heart failure and atrial fibrillation. Toxicity happens when levels go above 2 ng/mL, especially in people with kidney problems.
- Cancer drugs: Trastuzumab (Herceptin) can cause atrial fibrillation through inflammation and oxidative stress.
- Antiemetics: Ondansetron (Zofran) and domperidone - common for nausea - are known QT prolongers.
Here’s the kicker: it’s rarely just one drug. When you take two or more QT-prolonging medications together, your risk jumps 300% to 500%. That’s why polypharmacy - especially in older patients - is such a red flag.
Who’s Most at Risk?
Not everyone reacts the same way. Certain factors make you far more vulnerable:
- Age 65+: Over 60% of severe cases occur in older adults. Kidney function declines, drugs stick around longer, and electrolytes get harder to balance.
- Low potassium or magnesium: Hypokalemia affects 20% of hospitalized patients. Hypomagnesemia hits 10-15%. Both are silent triggers.
- Excessive alcohol: More than three drinks a day triples your risk. Alcohol depletes magnesium and directly irritates heart tissue.
- Genetics: About 15% of people of African ancestry carry the S1103Y variant. Around 12% of East Asians have the R1193Q variant. These make cells far more sensitive to QT-prolonging drugs. Testing for these is still rare - but it’s coming.
- Female gender: Women are more likely to develop torsades de pointes, even at lower drug doses.
And here’s something most people don’t realize: your heart doesn’t need a huge overdose to react. Sometimes, a normal dose - combined with a little dehydration, a missed meal, or a new supplement - is enough to tip the balance.
Warning Signs You Can’t Ignore
These symptoms don’t always mean you’re having a heart attack - but they’re your body’s alarm system:
- Palpitations: Feeling your heart flutter, race, or skip beats. Reported in 70-80% of cases.
- Dizziness or lightheadedness: Especially when standing up. This isn’t just “getting old.”
- Fatigue: Unexplained exhaustion, even after a full night’s sleep.
- Chest discomfort: Not always sharp pain. Sometimes just pressure, tightness, or a strange ache.
- Fainting or near-fainting: Syncope is a major red flag. If you’ve passed out after starting a new med, stop it and call your doctor - don’t wait.
Don’t dismiss these as stress or anxiety. If you’ve recently started a new medication - even if it’s been a few days - and you’re feeling off, it could be your heart.
How Doctors Manage Drug-Induced Arrhythmias
Management isn’t one-size-fits-all. It depends on the drug, the rhythm, and your overall health.
Step 1: Stop or adjust the medication. In 75-85% of cases, simply lowering the dose or switching to a safer alternative resolves the problem. For example, if metoprolol causes bradycardia, reducing the dose helps 60-70% of patients. If it doesn’t, and symptoms persist, a pacemaker might be needed.
Step 2: Correct electrolytes. If your potassium is below 4.0 mEq/L or magnesium under 2.0 mg/dL, your doctor will likely give you supplements - sometimes IV, especially if you’re symptomatic. This isn’t just a band-aid; it’s essential for stabilizing your heart’s electrical activity.
Step 3: Monitor with ECGs. Before starting high-risk drugs, you should get a baseline ECG. Then, another one within 72 hours. This catches QT prolongation early. For drugs like amiodarone or fluoroquinolones, repeat ECGs every few days during the first week are standard.
Step 4: Advanced interventions. For persistent cases, catheter ablation fixes the problem in 5-10% of patients. Surgery? Less than 2%. But those are last resorts.
And here’s the good news: if caught early, most drug-induced arrhythmias reverse completely. No permanent damage. No lifelong meds. Just a change in treatment plan.

What You Can Do Right Now
You don’t need to wait for a doctor’s visit to protect yourself. Here’s what works:
- Know your meds. Ask your pharmacist: “Could this cause heart rhythm problems?” Keep a list of everything you take - including supplements and OTC drugs.
- Check your electrolytes. If you’re on diuretics or have kidney issues, ask for a simple blood test to check potassium and magnesium. Don’t assume they’re fine.
- Limit alcohol and caffeine. Alcohol is a major trigger. Caffeine alone rarely causes serious arrhythmias, but it can make things worse if you’re already at risk.
- Stay hydrated. Dehydration worsens electrolyte imbalances. Drink water - especially if you’re sweating, sick, or on diuretics.
- Track symptoms. Write down when you feel palpitations, dizziness, or fatigue. Note what you took and when. This helps your doctor connect the dots.
And if you’ve had a family member who had sudden cardiac arrest or a history of unexplained fainting - tell your doctor. It might be genetic.
The Future: Personalized Medicine Is Here
Scientists aren’t just reacting - they’re predicting. Vanderbilt University used CRISPR-edited heart cells to show how specific gene variants make people more sensitive to drugs. That’s not science fiction - it’s the foundation of what’s coming.
The American College of Cardiology is rolling out a clinical tool in 2024 that calculates your personal risk before prescribing. It looks at your age, kidney function, current meds, electrolytes, and - if available - your genetic profile. Imagine walking into your doctor’s office and getting a risk score for your new antibiotic: “Low, Medium, or High.” That’s the future.
The FDA has added black box warnings to 25 drugs since 2010. That’s not bureaucracy - it’s protection. And in 2022 alone, they added eight more. The message is clear: this is a growing, recognized threat.
Experts predict a 30-40% drop in severe cases over the next five years - not because drugs are safer, but because we’re finally learning how to use them smarter.
Bottom Line
Medications save lives. But they can also trigger deadly heart rhythms - often without warning. The key isn’t avoiding meds. It’s knowing the signs, asking the right questions, and working with your doctor to stay safe. If you’re on any of the high-risk drugs listed here - or if you’ve had unexplained dizziness, palpitations, or fainting - don’t wait. Talk to your provider. Get an ECG. Check your electrolytes. Your heart might be sending you a message.
Can over-the-counter medications cause heart arrhythmias?
Yes. Common OTC drugs like pseudoephedrine (in cold and allergy meds), diphenhydramine (Benadryl), and some herbal supplements (like licorice root) can prolong the QT interval or trigger palpitations. Even high doses of caffeine from energy drinks or weight-loss pills can be risky, especially if you’re already on other medications or have underlying heart conditions.
If I feel heart palpitations after starting a new drug, should I stop taking it?
Don’t stop cold turkey unless you’re fainting, having chest pain, or struggling to breathe. Instead, call your doctor or pharmacist immediately. Some drugs, like beta-blockers or antiarrhythmics, need to be tapered. Stopping suddenly can cause rebound effects that are just as dangerous. Keep a symptom log and note when the palpitations started and what else you took that day.
Are there blood tests to check for risk before taking a medication?
Routine genetic testing isn’t standard yet, but doctors often check electrolytes (potassium, magnesium) and kidney function before prescribing high-risk drugs. An ECG is the most common tool to screen for QT prolongation. If you have a strong family history of sudden cardiac death or unexplained fainting, ask about genetic screening - some hospitals now offer it for high-risk patients.
Can diet help prevent drug-induced arrhythmias?
Absolutely. A diet rich in potassium (bananas, spinach, sweet potatoes) and magnesium (nuts, seeds, whole grains) helps stabilize heart rhythms. Avoid excessive salt, which worsens fluid retention and strains the heart. Limit alcohol - even moderate drinking increases risk by 200-300%. Staying well-hydrated and eating balanced meals reduces the chance of dangerous electrolyte drops.
Is it safe to take supplements with my heart medication?
Many supplements interact dangerously. St. John’s Wort can reduce effectiveness of blood thinners and beta-blockers. Licorice root lowers potassium and can trigger arrhythmias. Coenzyme Q10 is generally safe but can interfere with warfarin. Always tell your doctor about every supplement you take - even if you think it’s “natural.”



Sazzy De
January 31, 2026 AT 11:55Been on amiodarone for a year now and never knew it could cause the very thing it was supposed to fix. My doc never mentioned the QT risk. Just told me to take it and call if I felt weird. Guess I’m lucky I didn’t pass out at the grocery store.
Lily Steele
February 1, 2026 AT 10:08I’m a nurse and I see this all the time. Elderly patients on 7+ meds, no one checking electrolytes, and everyone blames the heart for being ‘old.’ It’s not aging-it’s polypharmacy. We need better systems.
Beth Beltway
February 2, 2026 AT 18:25Of course you’re at risk if you’re popping Benadryl like candy and drinking wine while on antidepressants. This isn’t rocket science. Stop being careless and take responsibility for your own health. It’s not the drug’s fault you’re a walking pharmacology experiment.
Kelly Weinhold
February 4, 2026 AT 08:17Hey I just wanted to say you’re not alone if you’ve had weird heart flutters after starting something new. I was terrified when I got dizzy after Zofran-thought I was dying. Called my pharmacist and they said ‘oh yeah that’s a known one’ and switched me to something else. Took 5 minutes. No big deal. You’re not crazy, your body’s just talking. Listen to it.
Rob Webber
February 6, 2026 AT 01:25They say 100k hospitalizations a year from meds. That’s not a side effect. That’s a systemic failure. Why aren’t pharmacists doing mandatory ECG reviews before dispensing QT-prolonging drugs? Why is this still on the patient to figure out?
calanha nevin
February 7, 2026 AT 02:06For those asking about supplements: St. John’s Wort is a silent killer with SSRIs. Licorice root is worse than you think. Even magnesium supplements can interact with diuretics. Always cross-check with your pharmacist. They’re not just the people who hand you pills-they’re your safety net.
Lisa McCluskey
February 8, 2026 AT 07:07My mom had torsades after a course of azithromycin. She didn’t even know it was an antibiotic. Took her a week to connect the dots. Now she keeps a printed list of every med she takes, including OTC. Simple. Effective. Everyone should do this.
owori patrick
February 8, 2026 AT 13:22In Nigeria we don’t have easy access to ECGs or electrolyte tests. But we know when someone feels off after a new medicine. We say ‘this one is not good for the heart’ and stop it. Sometimes the oldest wisdom is the most accurate. Listen to your body before you listen to the label.
Claire Wiltshire
February 9, 2026 AT 10:59It’s worth noting that the FDA’s black box warnings are not merely bureaucratic-they represent a hard-won recognition of iatrogenic harm. The fact that eight new drugs received such warnings in 2022 alone suggests a growing awareness that safety must precede convenience. We are moving in the right direction, albeit slowly.
April Allen
February 9, 2026 AT 15:36The pathophysiology here is fascinating-drug-induced QT prolongation is essentially a disruption of the repolarization phase of the cardiac action potential, primarily via hERG potassium channel blockade. The clinical implication is that even subtherapeutic plasma concentrations, when combined with hypomagnesemia or CYP3A4 inhibition, can precipitate torsades. This isn’t just pharmacology-it’s electrophysiological vulnerability amplified by polypharmacy.
Sheila Garfield
February 10, 2026 AT 17:39I took Zofran for nausea after chemo and got this weird fluttery feeling. Didn’t think much of it. Then I read this and realized it was probably the drug. Changed to a different one and it vanished. So simple. Why isn’t this common knowledge?
Shawn Peck
February 12, 2026 AT 09:48They’re gonna make us all wear heart monitors just to get a cold pill. Next thing you know, you’ll need a prescription to breathe. This is medical overreach disguised as safety.
Jason Xin
February 13, 2026 AT 14:00Oh so now we’re blaming the meds again? Funny how every time someone feels weird, it’s the drug’s fault. Maybe it’s stress. Maybe it’s coffee. Maybe you’re just anxious. I’ve been on 12 meds and my heart’s fine. Just saying.
Kathleen Riley
February 14, 2026 AT 12:16One might posit that the true ethical dilemma lies not in the pharmacological mechanism, but in the epistemic asymmetry between the patient and the prescriber. The patient, armed with incomplete information, becomes the unwitting experimental subject in a system that prioritizes efficiency over individualized risk assessment. This is not medicine-it is algorithmic negligence.