Hepatic Encephalopathy Explained – What You Need to Know
If you’ve ever felt unusually confused or had trouble concentrating, it might be more than just stress. In some people a damaged liver sends waste into the bloodstream that clouds the brain. That condition is called hepatic encephalopathy (HE). Knowing why it happens and how to act can keep your mind sharp.
Why the Liver Affects Your Brain
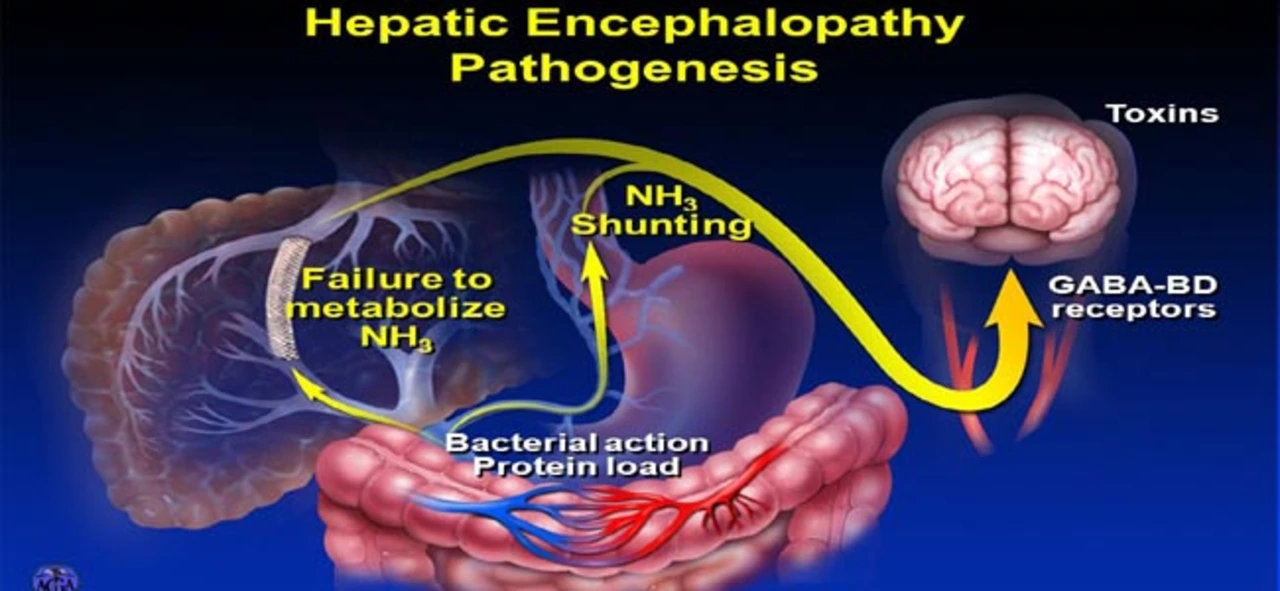
The liver’s job is to clean blood by turning harmful substances into safe ones. When liver cells are scarred or inflamed – as in cirrhosis, hepatitis, or fatty‑liver disease – they can’t filter out ammonia and other toxins. Those chemicals travel up to the brain, change nerve signaling, and produce mental slowness, personality shifts, or even coma.
Ammonia is the main culprit, but other substances like manganese also play a role. Medications that affect gut bacteria (for example certain antibiotics) can raise toxin levels too. That’s why doctors look at both liver health and what you’re taking when they suspect HE.
Spotting the Signs and Getting Help
HE shows up in stages. Early signs are subtle: forgetfulness, trouble with numbers, or a shaky hand. As it progresses, people may become disoriented, have slurred speech, or show unusual sleep patterns (like sleeping all day). The most severe stage can lead to stupor or coma.
Because symptoms overlap with many other conditions, the safest move is to get checked by a doctor if you notice any change in thinking that lasts more than a few days. Blood tests for ammonia levels and imaging of the liver help confirm the diagnosis.
When HE is caught early, treatment can reverse most symptoms within days. The key is to lower toxin production and improve how the gut handles waste.
Lactulose is a sugar‑based medicine that pulls ammonia into the colon where it’s expelled. Most patients start with a small dose that you adjust until you have two soft stools per day. Rifaximin, an antibiotic, cuts down harmful bacteria that create ammonia. Many doctors prescribe both together for better results.
Beyond pills, diet matters. Eating moderate protein – not too high, not too low – helps the liver without feeding toxin‑producing bacteria. Some find that splitting protein across meals reduces brain fog. Avoiding alcohol completely is non‑negotiable; even a small drink can trigger HE.
Staying hydrated and getting enough fiber keeps bowel movements regular, which also lowers ammonia buildup. If you’re on diuretics for fluid retention, talk to your doctor about balancing electrolytes so the treatment stays effective.
In advanced cases where medicines don’t keep symptoms at bay, a liver transplant may be the only long‑term solution. Until then, regular follow‑ups and monitoring ammonia levels guide dosage tweaks.
Here are three quick actions you can take today if you suspect HE:
- Call your healthcare provider and describe any new confusion or personality changes.
- Stop drinking alcohol and limit high‑protein snacks until you get medical advice.
- Make sure you’re drinking enough water and eating balanced meals with fiber.
Remember, HE is reversible for most people when caught early. Paying attention to mental shifts, keeping your liver healthy, and following treatment plans can keep your brain clear and life on track.