Doctors prescribe generics more than ever-90% of all prescriptions in the U.S. are for generic drugs as of 2023. But even with that number, many physicians still hesitate. Why? Because patients ask questions. And too often, doctors don’t have the right tools to answer them quickly, clearly, and confidently.
Why Generic Medications Still Feel Risky to Some Prescribers
It’s not that doctors don’t want to save patients money. They do. But the fear isn’t about cost-it’s about uncertainty. Is the generic really the same? Will it work for my diabetic patient who’s been on the brand for years? What if they have a bad reaction? These aren’t irrational concerns. They’re rooted in real gaps in education. A 2023 survey found that 52% of primary care doctors felt unprepared to explain bioequivalence to patients. Even worse, 38% admitted they sometimes default to brand-name drugs just to avoid the conversation. The FDA’s Generic Drugs Education Program, launched in 2008 and expanded under the GDUFA in 2012, was created to fix this. But awareness is low. Only 48% of physicians knew about the FDA’s Generic Drugs Stakeholder Toolkit-even though it’s free, updated regularly, and packed with ready-to-use materials.What the FDA Actually Says About Generic Equivalence
The science is clear: a generic drug must deliver the same active ingredient, in the same strength, and at the same rate as the brand-name version. The FDA requires proof through bioequivalence studies-testing in 24 to 36 healthy volunteers to show the drug’s absorption falls within 80% to 125% of the brand’s. That range isn’t a loophole. It’s a scientifically validated window. Think of it like this: two different brands of ibuprofen might absorb slightly differently, but both will lower your fever the same way. The same applies to statins, antibiotics, blood pressure meds. The FDA’s 2022 infographic, What Makes a Generic the Same as a Brand-Name Drug?, breaks this down visually. It shows side-by-side comparisons of how both versions are manufactured, tested, and monitored. And here’s the kicker: in 2022, the FDA analyzed over 12,000 adverse event reports for generics-just 635 more than for brand-name drugs. That’s not a red flag. That’s proof of equivalent safety.Tools That Actually Work in a Busy Clinic
Doctors don’t need a 40-page white paper. They need a 1-page handout they can grab during a 10-minute visit. The FDA’s Prescriber Flyers-available in both English and Spanish-are designed exactly for that. Printed on standard letter paper, they fit in office literature racks. Version 2 (released March 2022) includes QR codes linking to Spanish-language resources, addressing a key equity gap: 42% of Hispanic patients express higher concerns about generic quality than non-Hispanic patients. But the real game-changer? The Stakeholder Toolkit. It includes:- 12 ready-to-post social media templates for patient education
- 5 customizable info cards you can print and leave on the counter
- 3 infographics, including one that compares brand and generic manufacturing standards
Why Some Doctors Still Don’t Use These Resources
The biggest barrier? Time. A 2022 study in Annals of Internal Medicine found 73% of physicians said they simply don’t have time to look up generic drug info during a patient visit. Another 68% said the FDA flyers were “useful but too technical” for quick reference. And here’s the irony: most EHR systems don’t integrate these resources. Only 37% of major platforms like Epic or Cerner have pop-ups or alerts that bring up FDA generic info when a brand-name drug is selected. That’s changing. In July 2023, the FDA launched an API pilot that pushes real-time generic equivalence data directly into EHRs. Early results? A 15.2% increase in generic prescribing among participating doctors in just six months. Kaiser Permanente saw similar results after embedding FDA materials into their Epic system. They cut brand-name prescribing by nearly 19% in six months-without changing any formulary rules.How to Talk to Patients About Switching to Generics
Patients don’t trust generics because they’re cheap. They trust them when they understand why they’re safe. The FDA provides ready-made scripts for common objections:- Patient: “My doctor said the brand works better.”
Response: “The FDA requires generics to be identical in how they work in your body. The only difference is the inactive ingredients-which don’t affect how the medicine works.” - Patient: “I’m worried about side effects.”
Response: “We’ve tracked over 12,000 reports of side effects from generics last year. The number is almost the same as for brand-name drugs. That’s because they’re held to the same standard.” - Patient: “I’ve been on this brand for 10 years.”
Response: “Switching won’t change your results. The generic has the same active ingredient, same dose, same effect. The only thing that changes is your out-of-pocket cost.”
Cost Isn’t Just a Number-It’s a Treatment Barrier
The American College of Physicians says 20% to 30% of new prescriptions are never filled because of cost. For patients earning under $25,000 a year, that number jumps to 3.7 times higher. A 2023 JAMA Internal Medicine commentary put it plainly: switching from a $300/month brand-name drug to its generic saves the patient $262.50 a month. That’s $3,150 a year. That’s not a savings. That’s a lifeline. Dr. Janet Woodcock, former head of the FDA’s drug center, testified in 2021 that misconceptions about generics cost the U.S. healthcare system $1.3 billion annually in unnecessary brand-name use. Doctors who use these education tools don’t just save money-they save lives. Patients who can afford their meds are more likely to take them. And adherence is the single biggest predictor of health outcomes.What’s Missing-and What’s Coming Next
The biggest gap? Complex generics. Inhalers, topical creams, injectables-these aren’t as straightforward as pills. Bioequivalence is harder to prove. Only 42% of prescribers feel confident prescribing biosimilars, and 61% are confused about “authorized generics” (brand-name drugs sold under a generic label). New tools are emerging. IBM Watson Health tested an AI system in 2023 that generated personalized generic substitution recommendations based on a patient’s history, concerns, and insurance. In a trial with 120 doctors, patient acceptance of generics jumped by 29 percentage points. And the federal government is pushing harder. The 2024 Medicare Part D proposed rule includes financial incentives for plans that train prescribers on therapeutic alternatives. That could affect 49 million beneficiaries.What You Can Do Today
You don’t need to wait for EHR updates or AI tools. Start now:- Download the FDA’s Generic Drugs Stakeholder Toolkit (it’s free, no login needed).
- Print the Prescriber Flyer and keep it by your computer.
- Use the info cards in your exam rooms-patients read them while waiting.
- Practice the scripts. Say them out loud. You’ll sound more confident.
- Track your own prescribing rate. Compare it to your peers. You might be surprised.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence-meaning they deliver the same amount of medicine into the bloodstream at the same rate. Studies show generics work just as well in real-world use. In fact, 90% of all prescriptions filled in the U.S. are for generics.
Why do some patients refuse to take generics?
Many patients believe generics are cheaper because they’re lower quality. This misconception is often fueled by marketing, misinformation, or past experiences with inconsistent supply. Some patients also worry about switching from a medication they’ve used for years. The key is addressing these fears with clear, simple facts-like showing them the FDA’s infographic comparing manufacturing standards or explaining that the same inspectors check both brand and generic factories.
Is there a difference between generic and brand-name manufacturing?
No, not in terms of standards. Both are made in FDA-inspected facilities using the same quality controls. In fact, many brand-name companies also make their own generics under different labels. The FDA inspects all manufacturing sites-whether they make brand or generic drugs-with the same rigor. The only difference is the packaging and inactive ingredients, which don’t affect how the drug works.
What should I do if a patient says their generic doesn’t work?
First, don’t assume it’s the drug. Ask if they’re taking it as prescribed, if their insurance changed, or if they’re using a different pharmacy. Sometimes, switching pharmacies leads to a different inactive ingredient, which can affect absorption in rare cases. If the issue persists, check if it’s an authorized generic or a different manufacturer. Most of the time, the problem isn’t efficacy-it’s perception. Use the FDA’s patient scripts to explain how generics are tested and approved.
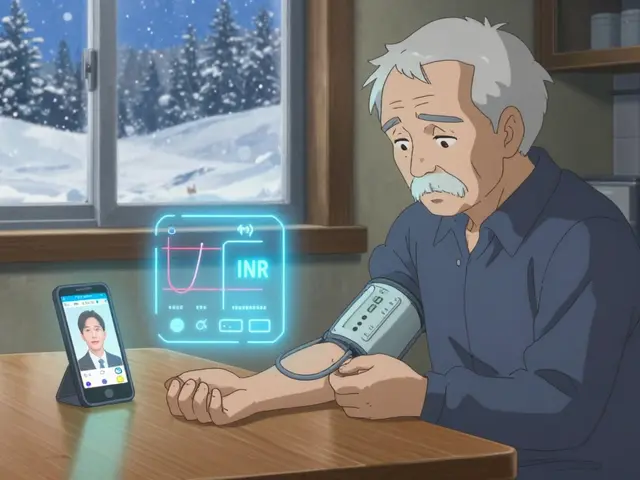
Can I trust generics for chronic conditions like high blood pressure or diabetes?
Absolutely. Generics are used daily for hypertension, diabetes, cholesterol, depression, and more-with the same success rates as brand-name drugs. Studies tracking patients on generic statins, metformin, and lisinopril show no difference in outcomes over years of use. The FDA monitors adverse events closely-over 12,000 reports were reviewed for generics in 2022, with results nearly identical to brand-name drugs.
Why aren’t these resources built into my EHR system?
Most EHRs haven’t integrated FDA resources yet-only 37% have pop-ups or alerts. But that’s changing. The FDA launched an API pilot in 2023 that connects generic drug data directly to Epic and Cerner. Early results show a 15% increase in generic prescribing among doctors using it. Ask your EHR vendor if they plan to add FDA generic education tools. You can also download the materials and create your own custom alerts.
Do generics have different side effects than brand-name drugs?
The active ingredient is identical, so the core side effects are the same. Sometimes, different inactive ingredients (like fillers or dyes) can cause rare reactions in sensitive patients-but this is uncommon. If a patient reports a new side effect after switching, it’s worth investigating, but it’s rarely because the generic is less safe. The FDA tracks all reports equally, and data shows no significant difference in safety profiles between brand and generic versions.
Are there any drugs where generics aren’t recommended?
For most drugs, generics are equally effective. But for some complex formulations-like inhalers, topical creams, or injectables-bioequivalence is harder to prove. These are called complex generics, and they require more careful evaluation. The FDA still approves them, but prescribers should be more cautious. For these, it’s best to stick with the same manufacturer unless there’s clear evidence of equivalence. Always check the FDA’s list of approved generics for complex drugs before switching.


Lauren Wall
January 20, 2026 AT 20:02Doctors who still hesitate on generics are either lazy or scared of a 30-second conversation. The science is settled. The FDA doesn’t mess around. If you can’t explain this to a patient, maybe you shouldn’t be prescribing.
Stop hiding behind ‘I don’t have time.’ Your patients don’t have time for overpriced meds either.
Kenji Gaerlan
January 22, 2026 AT 07:05lol why do u guys care so much about generics? i mean, if i pay for the brand, i get the brand. why risk it? also, my cousin took a generic and got like… weird dreams? idk man. maybe it’s the fillers. or the ghosts in the pill.
Daphne Mallari - Tolentino
January 24, 2026 AT 05:53While the FDA’s regulatory framework is undeniably robust, the persistent cognitive dissonance among prescribers reflects a deeper epistemological failure in medical education. The conflation of bioequivalence with therapeutic equivalence, though statistically valid, fails to account for interindividual pharmacokinetic variance-a nuance rarely addressed in continuing medical education.
Furthermore, the assertion that ‘90% of prescriptions are generic’ obscures the fact that many of these are prescribed under duress due to insurance formularies, not clinical confidence. The data is not the issue; the narrative is.
Neil Ellis
January 24, 2026 AT 17:38Man, I love this post. It’s like someone finally handed us the flashlight in a dark room we’ve been bumping into for years.
That infographic? I printed it. Laminated it. Taped it to my stethoscope. Patients now ask me, ‘Hey, is that the one with the FDA seal?’ And I just nod like a proud dad.
One lady cried when she saw the cost difference-$262 a month? That’s her rent. Her groceries. Her kid’s shoes. We’re not just talking pills here. We’re talking dignity.
And the API pilot? That’s the future. Imagine a world where your EHR whispers, ‘Hey, this brand has a generic that’s identical and saves them $250.’ No more guesswork. Just good medicine.
Let’s make this the new normal. Not because we have to. But because we can.
Alec Amiri
January 26, 2026 AT 09:07Oh wow, another ‘trust the FDA’ sermon. Let me guess-next you’ll say vaccines are fine and sunscreen doesn’t cause cancer?
My grandma took a generic blood pressure med and ended up in the ER. Turns out, the fillers made her allergic. The brand? Zero issues for 8 years.
So yeah, I’ll stick with the brand. And if you’re gonna judge me for it, go ahead. I’ve got a $300 co-pay and a 72-year-old who still walks her dog. You? You’ve got a PowerPoint.
Chiraghuddin Qureshi
January 28, 2026 AT 01:34Bro, this is fire 🔥
My uncle in Mumbai takes generic metformin for 10 years-no issues, saves him 90%.
And yeah, the FDA seal? Same as US. Same factory standards.
Stop overthinking. Trust science. 🙌
Also, the QR code on the flyer? Genius. My mom used it to show her friends. Now they all switch. 😎
Patrick Roth
January 29, 2026 AT 08:39Actually, the 80-125% bioequivalence range is a massive loophole. It means a generic can be 25% weaker OR 25% stronger than the brand. That’s not ‘the same.’ That’s a gamble.
And the FDA’s ‘12,000 adverse event reports’? That includes every sneeze and headache reported by anyone who took a pill. Correlation ≠ causation, folks.
Also, why are we assuming all patients want generics? Some don’t. Some need consistency. Some are scared. And guess what? That’s okay.
Stop pushing ideology. Start listening.
Ryan Riesterer
January 30, 2026 AT 01:32The core issue isn’t education-it’s system integration. The FDA toolkit is comprehensive, but its utility is functionally null in environments where clinical workflow is constrained by EHR latency, documentation burden, and cognitive load.
Without embedded decision support-real-time, context-aware, and interoperable-the resource set remains a theoretical intervention. The API pilot is the only meaningful step forward. All other efforts are frictionless noise.