Infected Abrasion Checker
Redness
Is the area around the wound red and spreading?
Warmth
Does the wound feel warmer than surrounding skin?
Pus/Fluid
Is there yellow/green discharge from the wound?
Systemic Symptoms
Do you have fever or feel unwell?
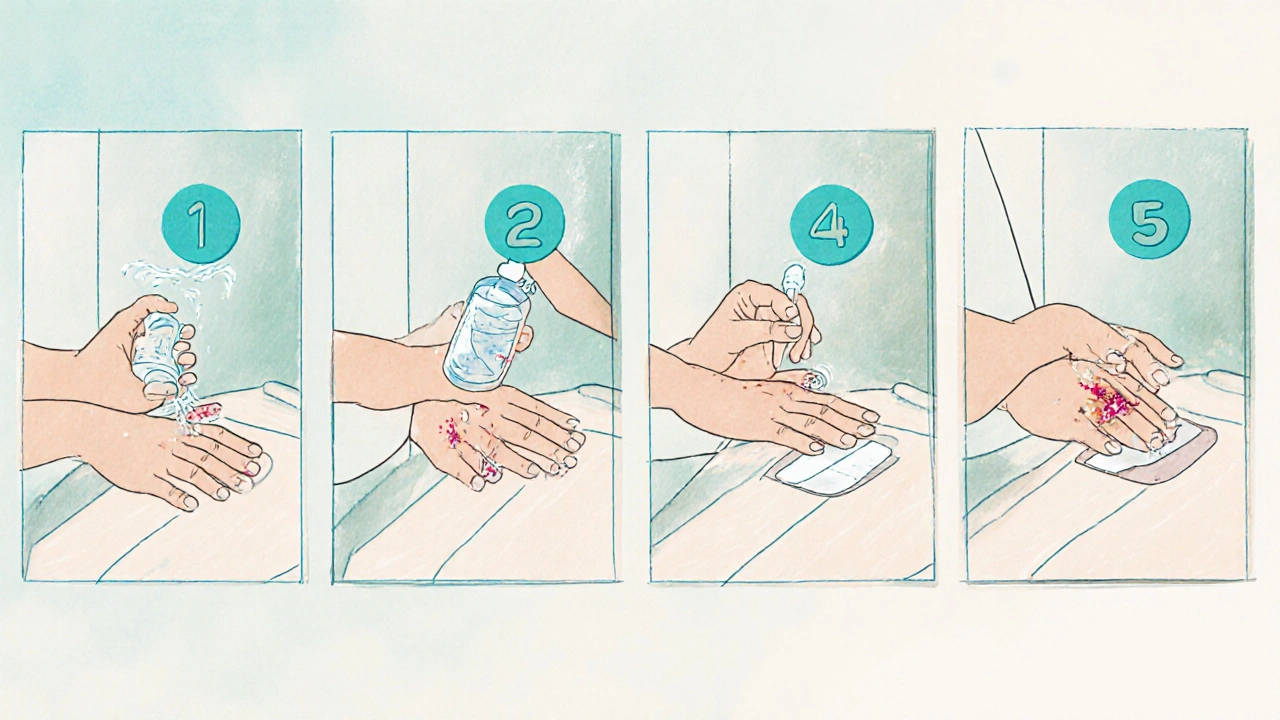
Treatment Steps
If the check indicates a possible infection, follow these steps:
- Wash hands thoroughly with soap and water.
- Rinse the wound gently with saline solution or clean water.
- Apply a thin layer of antibiotic ointment (e.g., Neosporin).
- Cover with a sterile, non-stick dressing.
- Change the dressing daily or when it gets wet/dirty.
Seek medical attention if symptoms worsen or persist beyond 5 days.
When a scrape turns red, painful, or starts oozing, it’s more than just a scrape - it could be an infected abrasion. Knowing the warning signs and the right steps to clean and treat the wound can stop a minor injury from becoming a serious problem.
Quick Take
- Redness, warmth, swelling, or pus = possible infection.
- Clean with saline, then apply an antibiotic ointment.
- Cover with a sterile dressing; change daily.
- Seek medical help if fever, spreading redness, or worsening pain.
- Keep tetanus shots up to date and avoid contaminating the wound.
What Actually Happens When an Abrasion Gets Infected?
Abrasion wounds remove the skin’s protective barrier, exposing the underlying tissue to the environment. Most of the time, the body’s natural defenses and proper cleaning keep bacteria at bay. But when Infected Abrasion is a wound that becomes colonized by harmful microorganisms, causing inflammation and tissue damage occurs, the immune response goes into overdrive.
The most common culprits are Bacteria that thrive on skin, especially Staphylococcus aureus and Streptococcus pyogenes. These microbes produce toxins that attract white blood cells, leading to redness, swelling, heat, and sometimes pus.
Spotting the Signs: How to Identify an Infected Abrasion
Early detection saves time and prevents complications. Look for these five hallmarks:
- Increasing Redness: A red halo that spreads beyond the wound’s edge.
- Warmth: The area feels hotter than surrounding skin.
- Swelling: Noticeable puffiness or a raised bump.
- Pus or Fluid: Yellowish or greenish discharge.
- Systemic Symptoms: Fever, chills, or feeling generally unwell.
If any of these appear within 24-48hours, treat the wound as potentially infected.
Step‑by‑Step First‑Aid: Cleaning and Treating at Home
Proper first‑aid stops bacteria from multiplying and gives the body a chance to heal.
-
Wash Your Hands. Use soap and warm water for at least 20seconds. This simple step cuts the chance of adding more germs.
-
Rinse the Wound. Gently flush the abrasion with Saline solution that is a sterile mixture of 0.9% sodium chloride, mimicking body fluids and minimizing tissue irritation. If you don’t have pre‑made saline, dissolve ½ teaspoon of salt in 1 cup of boiled‑then‑cooled water.
-
Remove Debris. Use a clean pair of tweezers to lift visible dirt or splinters. Avoid digging, which can tear tissue further.
-
Apply an Antibiotic Ointment. Choose an over‑the‑counter (OTC) option like bacitracin, neomycin (Neosporin), or polymyxin B (Polysporin). These ointments contain Antibiotic ointment that is a topical formulation designed to inhibit bacterial growth in superficial wounds. Use a thin layer; a thick coating can trap moisture and worsen infection.
-
Cover the Wound. Place a sterile non‑stick pad (e.g., Telfa) followed by a breathable adhesive bandage. This barrier keeps external contaminants out while allowing oxygen to reach the tissue.
-
Change Dressing Daily. Inspect the area each day. If the dressing becomes wet, damp, or dirty, replace it. Note any changes in color, odor, or amount of pus.
Continue this routine for up to a week. Most minor infections clear up within 5‑7days if treated promptly.
When Home Care Isn’t Enough: Signs You Need a Professional
Even with diligent first‑aid, some infections demand a clinician’s expertise. Seek medical help if you notice any of the following:
- Fever higher than 101°F (38.3°C) or chills.
- Redness expanding more than 2inches from the wound edge.
- Severe pain that isn’t relieved by OTC pain relievers.
- Rapid swelling, especially if it’s spreading to the surrounding joint.
- Pus that is thick, foul‑smelling, or changing color.
- Underlying health conditions (diabetes, immune suppression) that slow healing.
A Dermatologist is a medical professional specializing in skin health, capable of prescribing stronger topical or oral antibiotics and performing wound debridement when needed or your primary care physician can order a culture to identify the specific bacteria.
Prescription Options: What Doctors May Prescribe
If an infection is caused by resistant Staphylococcus aureus, a doctor might prescribe oral antibiotics such as dicloxacillin, cephalexin, or, for MRSA concerns, clindamycin. In some cases, a prescription‑strength topical like Mupirocin is used because it has a broader spectrum against Gram‑positive bacteria.
These medications work systemically (oral) or locally (topical) to inhibit bacterial protein synthesis, halting growth and allowing the immune system to clear the infection.
Comparing Common OTC Antibiotic Ointments
| Brand | Active Ingredient | Spectrum Coverage | Typical Price (USD) | Prescription Needed? |
|---|---|---|---|---|
| Bacitracin | Bacitracin zinc | Gram‑positive only | $4‑$6 | No |
| Neosporin (Neomycin) | Neomycin + polymyxin B + bacitracin | Broad (Gram‑positive & some Gram‑negative) | $5‑$8 | No |
| Polysporin | Polymyxin B + bacitracin | Gram‑positive & limited Gram‑negative | $5‑$7 | No |
Choose an ointment based on allergy history (neomycin can cause contact dermatitis) and the severity of the infection. For deep or rapidly spreading infections, skip OTC and see a clinician ASAP.
Preventing Infection Before It Starts
Prevention is cheaper than treatment. Follow these habits:
- Keep Tetanus Up‑to‑Date. Tetanus spores love dirty wounds; a booster every 10years is essential.
- Wear Protective Gear. Gloves, long sleeves, and proper footwear reduce the chance of abrasions.
- Clean Surfaces. If you’re working in a workshop, wipe down tools and floors regularly.
- Practice Good Hand Hygiene. Clean hands before handling any wound.
- Stay Hydrated and Eat Protein‑Rich Foods. Nutrition supports skin regeneration.
Common Pitfalls and How to Avoid Them
Even well‑intentioned people make mistakes that turn a simple scrape into an infection.
- Using Hydrogen Peroxide: It kills bacteria but also damages healthy cells, slowing healing.
- Applying Too Much Ointment: Moist environments invite anaerobic bacteria.
- Skipping the Dressing: Exposure to dirt and air accelerates contamination.
- Ignoring Allergic Reactions: Red rash and itching may mean the ointment itself is the problem.
Swap peroxide for sterile saline, apply a thin layer of ointment, and always cover the wound.
Recovery Timeline: What to Expect
Day1-2: Redness and mild pain are normal. Keep dressing clean.
Day3-5: If infection is responding, redness fades, swelling diminishes, and any pus becomes clearer.
Day6‑10: New skin forms. You may see a slight pink scar that fades over weeks.
If after ten days the wound hasn’t improved, schedule a medical review.
Frequently Asked Questions
Can I use honey to treat an infected abrasion?
Medical‑grade honey (like Manuka) has antibacterial properties and can be a safe adjunct for minor infections, but it should not replace proper cleaning and a certified antibiotic ointment. Always cover the honey with a sterile dressing.
How long should I keep a tetanus booster after a dirty scrape?
If your last booster was more than five years ago and the wound is dirty or deep, get a tetanus toxoid booster within 48hours. If you’re up to date (<10years), routine care is sufficient.
Is it safe to use antibiotic ointment on a child?
Yes, most OTC ointments are pediatric‑friendly, but avoid neomycin if the child has a known allergy. For infants under two months, consult a pediatrician before applying any medication.
What does a ‘foul‑smelling’ discharge indicate?
A foul odor suggests anaerobic bacterial growth, often linked to deeper tissue involvement. This scenario warrants prompt medical evaluation and possibly oral antibiotics.
Can I wash an infected abrasion with alcohol?
Alcohol is too harsh; it kills healthy cells and can worsen pain. Stick to sterile saline or clean water.




Judson Voss
October 1, 2025 AT 20:49Honestly, most people skim these kinds of guides and still end up with nasty infections because they ignore the basics. Hand washing isn’t optional, and you should treat any sign of pus like a red flag. If you’re not diligent about changing dressings, you’re practically inviting bacteria to set up camp.
Jessica Di Giannantonio
October 11, 2025 AT 04:01Wow, what a thorough rundown! I love how you laid out each step like a drama sequence – first the tension with the redness, then the triumphant rescue with the antibiotic ointment.
It really gives confidence that a simple scrape doesn’t have to turn into a nightmare.
RUCHIKA SHAH
October 20, 2025 AT 11:13Good info simple and clear. washing hands first then rinse use salt water if no saline. apply thin ointment and cover. change daily watch for spread. stay calm and follow steps.
Justin Channell
October 29, 2025 AT 17:25Got it! 🙌 wash hands, rinse well, thin layer of ointment, cover up 😊 change daily, keep an eye on redness and swelling.
Basu Dev
November 8, 2025 AT 00:37When dealing with an infected abrasion, the cascade of events that follows the breach of the epidermal barrier is both fascinating and critical to understand. The moment skin is compromised, resident flora and environmental microbes seize the opportunity to colonize the exposed tissue. This triggers an immediate innate immune response, recruiting neutrophils that release reactive oxygen species and proteolytic enzymes to fight the invaders. However, if the bacterial load overwhelms these defenses, a localized inflammatory milieu develops, manifesting as the classic signs of redness, warmth, swelling, and pus formation. At this stage, systemic symptoms such as fever may arise as cytokines enter the circulation, signaling that the body perceives a broader threat. Prompt mechanical cleaning with sterile saline reduces bacterial burden and removes debris that can shield pathogens from immune cells. Following irrigation, a thin layer of a broad-spectrum topical antibiotic, such as Neosporin, creates a chemical barrier that inhibits bacterial protein synthesis, further curbing replication. The choice of dressing matters; non‑stick, breathable gauze maintains a moist environment conducive to epithelial migration while preventing maceration. Daily dressing changes are essential not only to monitor the wound’s appearance but also to disrupt biofilm formation, a common cause of chronic infection. Throughout this process, nutrition and hydration play supportive roles, supplying the substrates needed for collagen synthesis and immune cell function. If after 48‑72 hours the wound shows no improvement-persistent erythema, expanding edema, or increasing purulence-systemic antibiotics may be warranted, guided by culture results when possible. In cases where the patient has comorbidities like diabetes or immunosuppression, the threshold for seeking medical care should be lower, given the heightened risk of rapid deterioration. Ultimately, the combination of meticulous local care, vigilant observation, and timely escalation to professional treatment creates the best odds for a swift, uncomplicated recovery.
Krysta Howard
November 17, 2025 AT 07:49Look, the guide nails the essentials, but let’s cut the fluff – if you see pus turning green, don’t wait. Grab an OTC ointment, slap it on, and call your doctor if it doesn’t improve in a day. 😡 This isn’t a suggestion, it’s a must‑do for anyone who cares about staying healthy.
Elizabeth Post
November 26, 2025 AT 15:01I appreciate the clear step‑by‑step. It’s helpful to know exactly when a simple scrape needs a professional’s eye, especially for those of us who tend to overlook the small changes.
Brandon Phipps
December 5, 2025 AT 22:13The piece does a solid job of marrying practical advice with the science behind infection. It reminds me that excessive use of hydrogen peroxide is a common mistake; it can actually delay healing by killing the very cells we need for tissue repair. Also, the emphasis on tetanus boosters is spot‑on – many overlook that after a dirty scrape. Keeping a small first‑aid kit with saline, a gentle ointment, and a sterile dressing can make all the difference, especially for those who work outdoors. In the end, a balanced approach-cleaning, protecting, and monitoring-keeps the risk low and the recovery swift.
yogesh Bhati
December 15, 2025 AT 05:25hey folks, just a quick tip – i always keep a bit of honey on hand for minor wounds. it’s a natural antibactier and can help if you don’t have ointment. just make sure the dress is clean and change it often.
Akinde Tope Henry
December 24, 2025 AT 12:37While your honey hack might work for a few, it’s not a substitute for proper medical care. Those who value their health should stick to proven sterile methods.
Brian Latham
January 2, 2026 AT 19:49Meh, just another list.