Imagine being terrified to step outside because a single bee sting could send you to the hospital-or worse. For over 3 million Americans, this isn’t fear. It’s reality. Stinging insect allergies aren’t just annoying; they’re life-threatening. But there’s a proven, powerful solution: venom immunotherapy. Unlike epinephrine, which only reacts after a sting, venom immunotherapy changes how your body responds to venom-forever.
What Is Venom Immunotherapy?
Venom immunotherapy (VIT) is a treatment that slowly teaches your immune system to stop overreacting to insect venom. It’s not a cure, but it’s the closest thing we have. You get tiny, controlled doses of purified venom from bees, wasps, hornets, yellow jackets, or fire ants. Over time, your body learns not to see venom as a threat. This process is called desensitization. It’s been used since the 1970s, and today, it’s one of the most effective allergy treatments in medicine. Studies show it cuts the risk of a severe reaction after a sting from 40-70% down to just 3-15%. That’s a 90% drop in danger. For people who’ve had anaphylaxis from a wasp sting, this isn’t just helpful-it’s life-changing.How It Works: The Two Phases
VIT happens in two clear stages. The first is the buildup phase. You start with a dose so small it’s harmless-sometimes as little as 0.05 micrograms. You get shots once or twice a week, and each week, the dose increases. It takes 8 to 20 weeks to reach the full maintenance dose: 100-200 micrograms. This is the amount that gives you long-term protection. Once you hit that dose, you move to maintenance. You get a shot every 4 to 8 weeks, for at least 3 to 5 years. Some people need it longer, especially if they’ve had severe reactions in the past. The venom used isn’t random-it’s lab-made, FDA-regulated, and standardized. Each batch must be 95% consistent in potency. For honeybees, it’s Api m 1. For yellow jackets, it’s Ves v 5. For fire ants, it’s Sol i 3. These are the exact proteins that trigger your allergic response.Why It Works Better Than Epinephrine Alone
Epinephrine is essential. It’s the emergency tool that saves lives during a reaction. But it doesn’t stop the next one. VIT does. A 2022 review of 12 studies found that people who only carried epinephrine had a 48-65% chance of another severe reaction. Those on VIT? Only 3-15%. That’s not a small difference-it’s the difference between living in fear and living normally. Other approaches, like sublingual drops (placed under the tongue), exist. But they’re far less effective-only 40-55% success rate. Oral immunotherapy? Still experimental. No FDA-approved options yet. VIT is the only treatment proven to change your immune system’s memory. And it works best for vespid venom (wasps, hornets, yellow jackets)-with protection rates of 91-96%. For honeybees, it’s still strong at 77-84%.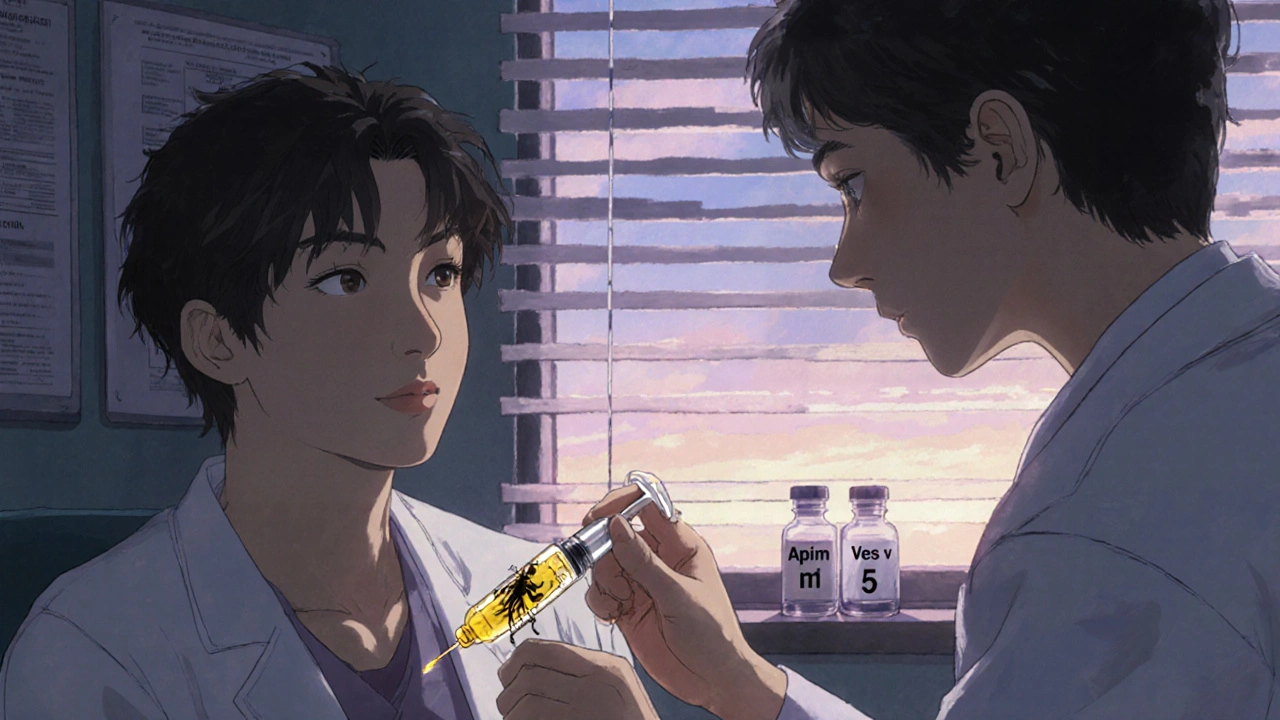
Who Should Get It?
Not everyone with a sting reaction needs VIT. The guidelines are clear. If you had symptoms beyond hives or swelling-like trouble breathing, dizziness, vomiting, or loss of consciousness-you’re a candidate. If you’ve had a reaction within minutes of being stung, you’re at high risk. So are people with mast cell disorders, outdoor workers, or anyone who spends time in gardens, parks, or campsites. Doctors use venom-specific IgE blood tests and skin tests to confirm the allergy. But here’s the catch: poor history-taking leads to 20-30% of wrong referrals. If you say, “I got swollen after a bee sting,” but didn’t have systemic symptoms, you might not need VIT. If you passed out? You absolutely do.Side Effects and Risks
VIT is safe, but it’s not risk-free. About 2-5% of people have a systemic reaction during treatment-usually mild: itching, hives, or mild breathing trouble. Severe reactions are rare. That’s why every shot is given in a doctor’s office, and you have to wait 45-60 minutes afterward. You can’t just drive off after the shot. Some people get redness or swelling at the injection site. That’s normal. Others miss work or school because of the frequent visits. But for most, the trade-off is worth it. A 2022 survey of over 1,200 VIT patients found 87% felt less anxious about outdoor activities. 73% stopped carrying multiple epinephrine pens. There’s one group where VIT is riskier: people with mastocytosis. Their bodies overproduce mast cells, which can make reactions harder to control. Even with VIT, their failure rate jumps to 15-20%. Doctors need to be extra careful here.Real People, Real Results
On Reddit’s r/Allergies, 89% of users who tried VIT said they’d recommend it. One woman wrote: “I used to panic every time I saw a wasp. Now I garden with my kids. I don’t carry three pens anymore.” A man on a patient forum said: “I started VIT after my first anaphylactic reaction. Two years later, I went hiking in the Rockies. I didn’t think I’d ever do that again.” The data backs this up. The VIT-QoL scale-a validated tool used in clinics-shows patients improve by an average of 1.21 points on a 7-point scale. That’s a major jump in daily life. Clinics offering VIT average 4.6 out of 5 stars on Yelp. The top reason? “Lifesaving.” The biggest complaint? Insurance.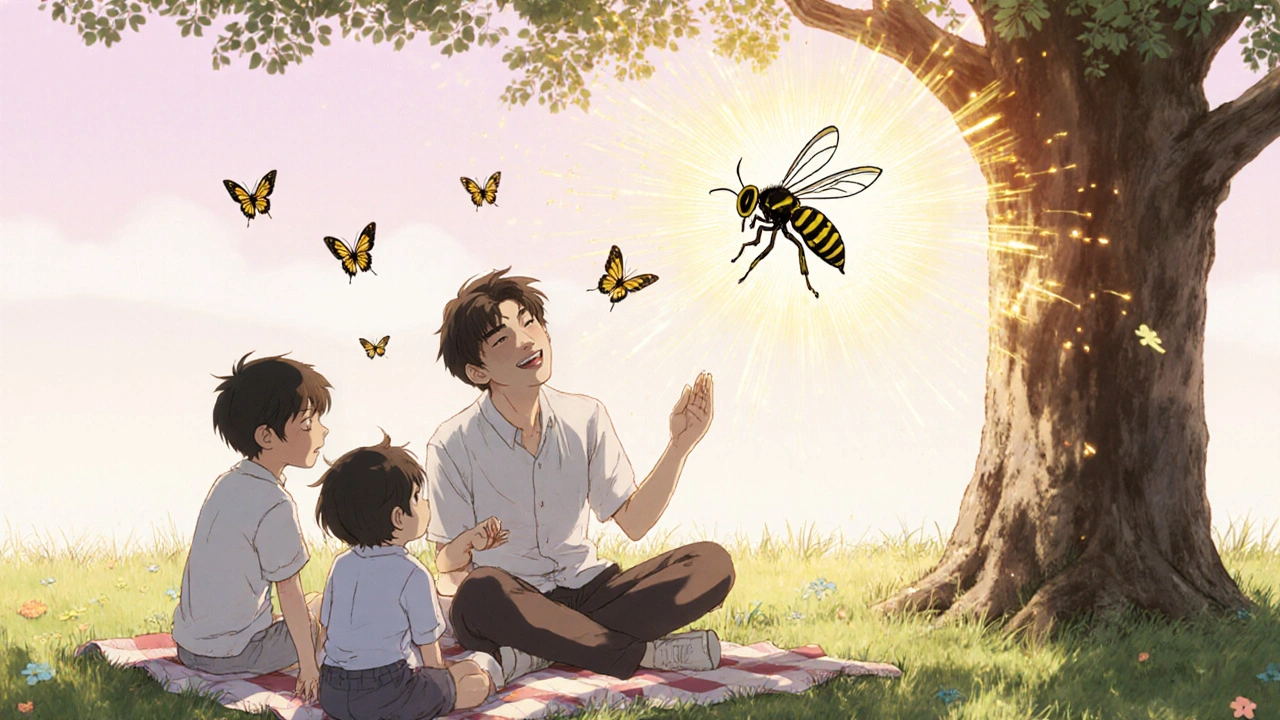
Cost, Access, and the Future
VIT isn’t cheap. Annual costs range from $2,800 to $4,500. Medicare covers 80% after your deductible. Private insurers approve 75-85% of requests-but only if you jump through hoops. Prior authorization? Usually required. Some patients pay out-of-pocket for months before getting coverage. There are only three major manufacturers: ALK-Abelló, Meridian Healthcare, and Diater. They supply nearly all the venom extracts in the U.S. And now, there’s a new option: a standardized fire ant venom extract approved by the FDA in January 2023. That’s good news for the 600,000 Americans allergic to fire ants. The biggest barrier? Access. One in three rural Americans live more than 50 miles from an allergist. That’s why VIT is still underused. Only 15% of the 3 million people who could benefit are actually getting it. The future looks promising. Rush protocols can get you to maintenance in just 1-3 days instead of months. But they come with a 35% higher chance of early reactions. Researchers are also testing recombinant venom proteins-made in labs, not extracted from insects. That could make treatments more consistent and safer.What Happens After You Stop?
You might wonder: “If I stop the shots, will the allergy come back?” For most people, no. Studies show 85-90% of patients stay protected for 5 to 10 years after stopping VIT. Some stay protected for life. That’s why doctors don’t rush to stop it. They wait until you’ve had at least 3-5 years of maintenance therapy. There’s one exception: if you have a mast cell disorder, or if you had a very severe reaction before treatment, your doctor might recommend staying on it longer-or even indefinitely.Final Thoughts: Is It Worth It?
Venom immunotherapy isn’t a quick fix. It takes time. It takes trips to the clinic. It takes patience. But if you’ve ever been terrified of a bee, a wasp, or a fire ant-this treatment gives you back your freedom. It’s the only therapy that doesn’t just treat the reaction. It treats the cause. The evidence is overwhelming. The success rates are among the highest of any allergy treatment. The cost-benefit ratio? One dollar spent on VIT saves $7.30 in emergency care. The quality of life gains? Measurable, real, and profound. If you’ve had a systemic reaction to a sting, talk to an allergist. Don’t wait for the next one. VIT isn’t just a treatment. For many, it’s the difference between living in fear-and living fully.Can venom immunotherapy cure a stinging insect allergy?
No, it doesn’t cure the allergy, but it changes how your immune system responds to venom. Most people develop long-lasting protection-often for 5 to 10 years after stopping treatment. Some stay protected for life. It’s the closest thing to a cure we have.
How long does venom immunotherapy take to work?
You start seeing protection during the buildup phase, but full protection usually takes 3 to 6 months. The real benefit comes after reaching the maintenance dose and continuing for at least 3 years. Most patients report feeling safer within the first few months.
Is venom immunotherapy safe for children?
Yes, but it’s less common. Only about 12% of VIT patients are under 18. Doctors are cautious because children’s reactions can be unpredictable, and long-term data is still growing. But for kids with severe reactions, VIT is recommended and can be very effective.
What if I have a reaction during treatment?
Reactions during VIT are rare and usually mild-like itching, swelling at the injection site, or mild hives. Serious reactions happen in 2-5% of patients. That’s why all shots are given in a clinic, and you must wait 45-60 minutes after each one. Staff are trained to handle reactions immediately.
Can I stop VIT if I feel better?
Don’t stop without talking to your allergist. Stopping too soon increases your risk of another severe reaction. Most patients stay on maintenance for 3-5 years. Even then, your doctor will check your IgG4 levels and review your history before deciding to stop. Many stay protected for years after stopping.
Does insurance cover venom immunotherapy?
Most insurance plans cover VIT, but you’ll likely need prior authorization. Medicare covers 80% after your deductible. Private insurers approve 75-85% of requests. Costs range from $2,800 to $4,500 per year. Some patients pay out-of-pocket for months before getting approval.
What insects does venom immunotherapy cover?
VIT works for honeybees, wasps, hornets, yellow jackets, and fire ants. Each has its own standardized venom extract. There’s no treatment for mosquitoes, ticks, or other biting insects-only stinging Hymenoptera. If you’re allergic to multiple types, you may need combination therapy.
How do I know if I’m a good candidate for VIT?
If you’ve had a systemic reaction to a sting-like trouble breathing, dizziness, vomiting, swelling in the throat, or loss of consciousness-you’re likely a candidate. Skin or blood tests confirm the allergy. If you only had hives or local swelling, VIT may not be needed. Talk to an allergist to review your history.





kora ortiz
November 17, 2025 AT 14:06After my first anaphylactic reaction, I thought I’d never garden again. VIT changed everything. I’m 2 years in, no more panic attacks when I hear a buzz. I carry one pen now, not three. This isn’t just medicine-it’s freedom.
Stop waiting for the next sting. Talk to an allergist. Now.
Jeremy Hernandez
November 18, 2025 AT 21:08Yeah right. Big Pharma’s latest money grab. They want you hooked on shots for 5 years so you keep paying. Epinephrine’s free at CVS. Why not just carry it and avoid bees like a normal person?
Also, how many people actually die from wasps? Like 3 a year? You’re more likely to get hit by lightning.
Also also-why do they use insect venom? Isn’t that kinda wild? What if they mix up the batches? I’d be scared to get this.
Tarryne Rolle
November 19, 2025 AT 15:36It’s interesting how we’ve turned nature’s defense mechanism into a medical problem to be ‘fixed.’
Is the real issue the venom-or our fear of mortality? We’ve built an entire industry around erasing discomfort, not learning to live with risk.
What if the allergy isn’t a flaw in your body, but a signal? A reminder that you’re alive, vulnerable, part of the ecosystem?
Maybe the real cure isn’t a shot-it’s acceptance.
But hey, if you want to pay $4k a year to feel safe, go ahead. I’ll be over here, letting the wasps do their thing.
Kyle Swatt
November 20, 2025 AT 04:57Let me tell you something real-this isn’t just about shots and venom. It’s about reclaiming your damn life.
I used to avoid picnics, BBQs, even walking my dog. My wife had to carry two EpiPens because I’d freeze like a deer in headlights every time a fly buzzed by.
VIT didn’t just lower my risk-it lowered my anxiety. Like, actual, soul-crushing fear. The kind that makes you cry in the grocery store because you saw a yellow jacket on a watermelon.
Yeah it’s a hassle. Yeah you gotta wait 45 minutes after every shot. But when you finally sit outside without checking the sky every 3 seconds? That’s not medicine. That’s magic.
And no, it’s not ‘Big Pharma.’ It’s science. Real, tested, FDA-approved science that’s saved thousands of us from becoming a statistic.
Don’t let the cynics scare you off. You deserve to live without fear.
Deb McLachlin
November 22, 2025 AT 03:25Thank you for this comprehensive overview. The data presented on success rates and quality-of-life improvements is compelling. I am particularly interested in the long-term durability of protection post-therapy, as well as the cost-effectiveness analysis. Could you clarify whether the $7.30 savings per dollar spent includes indirect costs such as lost productivity or caregiver burden? Additionally, are there any longitudinal studies tracking patient outcomes beyond 10 years post-treatment cessation?
saurabh lamba
November 24, 2025 AT 02:04bro why u pay so much money for shots when u can just use a fly swatter and chill
also i think u r scared of nature. why u not live in a box like robot?
in india we just slap bee and drink chai. no problem.
also is this like homeopathy but with needles? lol
Kiran Mandavkar
November 25, 2025 AT 08:57How dare you suggest this is ‘lifesaving’? You’re romanticizing medical intervention while ignoring the fundamental absurdity of treating a natural immune response as a disease.
This isn’t science-it’s cultural panic dressed in lab coats. The fact that 87% of patients feel ‘less anxious’ proves nothing but psychological dependency on institutional validation.
And let’s not pretend the venom extracts are ‘standardized.’ They’re extracted from insects-biological chaos in a vial. How can you trust purity when the source is inherently variable?
Meanwhile, real medicine is gene therapy and mRNA. This? This is 1970s band-aid thinking. Pathetic.
Eric Healy
November 27, 2025 AT 06:54My cousin got VIT and now she’s like ‘oh i just go outside’ like its no big deal
but i saw her doc’s office and the waiting room was full of people with epipens hanging off their bags like necklaces
kinda creepy honestly
also why do they use wasp venom? isnt that like feeding the monster?
Shannon Hale
November 28, 2025 AT 11:23OMG I’M CRYING. I had my first anaphylaxis at 19. I thought I’d die alone in a park. I carried 4 EpiPens. I wore a medical alert bracelet that said ‘DO NOT LET ME DIE.’
I started VIT 6 months ago. Last week, I sat under a tree with my niece and we watched bees pollinate flowers. I didn’t move. I didn’t flinch.
I didn’t cry. I just smiled.
THIS IS THE BEST THING THAT’S EVER HAPPENED TO ME.
TO THE DOCTORS WHO DO THIS WORK: YOU ARE ANGELS.
TO THE PEOPLE WHO THINK IT’S A SCAM: YOU’VE NEVER LIVED IN FEAR.
THIS ISN’T MEDICINE. IT’S A SECOND CHANCE.
Holli Yancey
November 29, 2025 AT 13:18I appreciate the depth of this post. I’ve been hesitant about VIT because of the time commitment, but reading these stories made me reconsider.
My dad had a reaction years ago and refused treatment. He’s fine now, but he still won’t go near any flowers. I wonder if he’d feel different now.
Maybe I’ll bring this to his next appointment.
Elia DOnald Maluleke
December 1, 2025 AT 04:35It is fascinating to observe the intersection of immunological science and human psychology. The notion that one can, through deliberate exposure, reprogram the body’s defensive mechanisms, speaks to the extraordinary plasticity of biological systems.
One cannot help but reflect on the broader implications: if the immune system can be trained to tolerate venom, might it also be trained to tolerate allergens, autoantigens, even societal anxieties?
There is a profound metaphor here-not merely of healing, but of transformation. To be taught, not to fear, but to coexist.
May we all, in our own ways, receive such a gift.
satya pradeep
December 2, 2025 AT 06:39u guys are overthinking this. i work in a field in india, get stung 3-4 times a year. i take antihistamine, chill, live.
but if u scared, go for shot. no judgment.
but dont make it sound like miracle. its just another treatment. not magic.
also, fire ant venom? we dont even know what that is here. we just call it ‘red ant pain’ and move on.
but if u need it, get it. ur life, ur call.