Asthma Trigger Risk Calculator
Your Asthma Risk Assessment
How This Works
Based on your answers, this tool estimates your risk level for asthma attacks using mechanisms explained in the article.
Ever wonder why a simple sneeze can turn into a choking, wheezing nightmare for someone with asthma? The answer lies in a cascade of events that happen inside the lungs in just seconds. Below we break down the science behind asthma attacks so you can spot the warning signs and understand what’s really going on.
What Exactly Is an Asthma Attack?
In plain terms, an asthma attack is a sudden worsening of asthma symptoms caused by rapid narrowing of the airways. This narrowing, called bronchoconstriction, makes it harder to move air in and out, leading to breathlessness, coughing, and that unmistakable wheeze.
The Chain Reaction: From Trigger to Symptom
Think of your airway as a flexible tube lined with delicate tissue. When a trigger-like pollen or a cold virus-hits, the body’s immune system jumps into action. Here’s the step‑by‑step rundown:
- Trigger particles land on the airway lining.
- Allergen‑specific IgE antibodies bind to mast cells that sit just under the surface.
- Mast cells release histamine and other chemicals.
- These chemicals cause the smooth muscle around the bronchi to contract-this is bronchoconstriction.
- Simultaneously, blood vessels become leaky, leading to airway inflammation.
- Inflammation attracts more immune cells, especially eosinophils, which release toxic proteins that further irritate the lining.
- The combined effect-tight muscles + swelling + mucus-drastically reduces airflow, and the attack hits.
All of this can unfold in under five minutes. No wonder the feeling is sudden and terrifying.
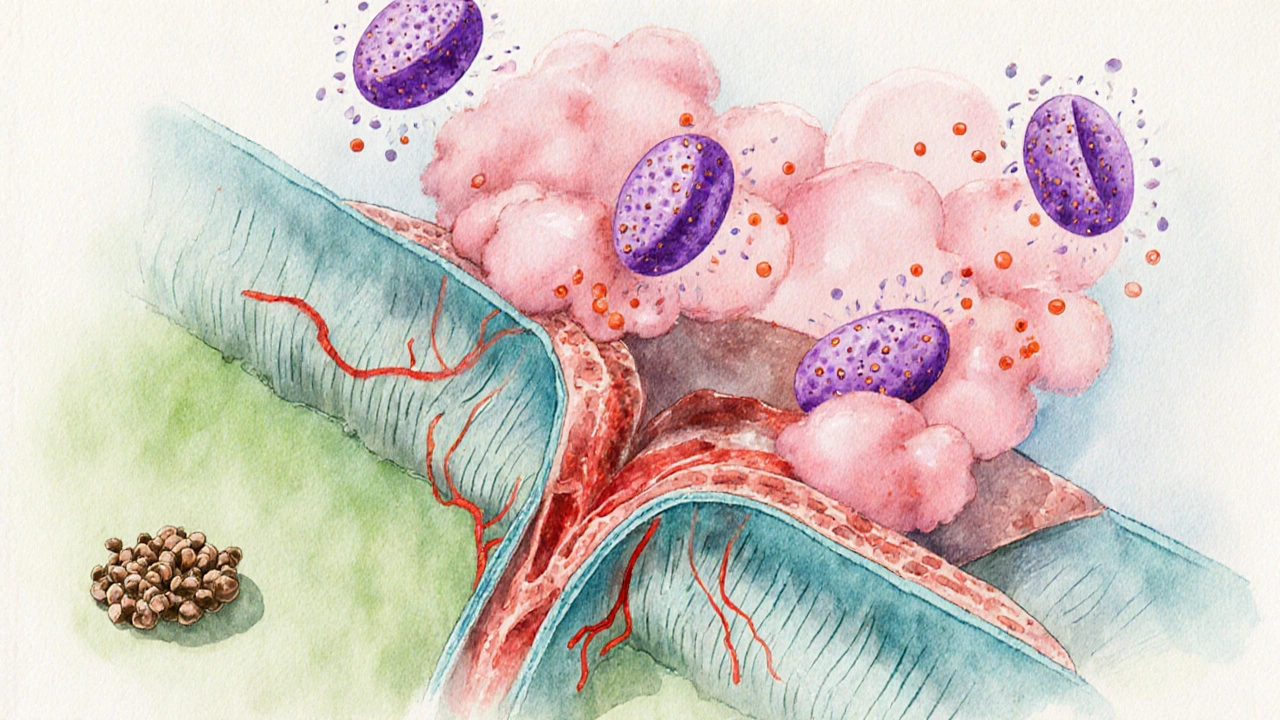
Key Players in the Airway
Understanding the main actors helps demystify why certain treatments work.
- Bronchoconstriction: The muscle tightening around the bronchi. Quick‑acting bronchodilators target this directly.
- Airway Inflammation: Swelling that narrows the passage. Inhaled corticosteroids aim to calm this over time.
- Mast Cells: Sentinels that release histamine and leukotrienes at the first sign of an allergen.
- Eosinophils: White blood cells that pile up in allergic asthma, releasing proteins that damage airway tissue.
- Cytokines (e.g., IL‑4, IL‑5, IL‑13): Chemical messengers that drive the allergic response and promote eosinophil survival.
- Bronchodilators: Medications like albuterol that relax airway muscles within minutes.
- Corticosteroids: Anti‑inflammatory drugs that reduce swelling and eosinophil activity over days to weeks.
Common Triggers and How They Spark the Reaction
| Trigger | Primary Mechanism | Typical Onset |
|---|---|---|
| Pollen (seasonal) | IgE‑mediated mast cell degranulation | Minutes to an hour |
| Viral respiratory infection | Increased airway inflammation & mucus production | Hours to days |
| Exercise (especially in cold air) | Bronchoconstriction from hyperventilation | During/after activity |
| Strong odors or pollutants | Direct irritation → reflex bronchoconstriction | Immediate |
| Stress or strong emotions | Neuro‑immune pathways trigger mast cells | Minutes |
Notice how many triggers converge on the same two mechanisms: muscle tightening and swelling. That’s why a single inhaler can often help across different situations.

Why Some Attacks Are Severe
Not all attacks are created equal. A few factors turn a mild flare‑up into a life‑threatening crisis:
- Bronchial hyperresponsiveness: The airways become overly sensitive, reacting to even low‑level irritants.
- High eosinophil count: More eosinophils = more tissue damage and mucus.
- Concurrent infection: Viruses can amplify inflammation and make bronchodilators less effective.
- Delayed treatment: Waiting even 5‑10 minutes to use a rescue inhaler lets the cascade run unchecked.
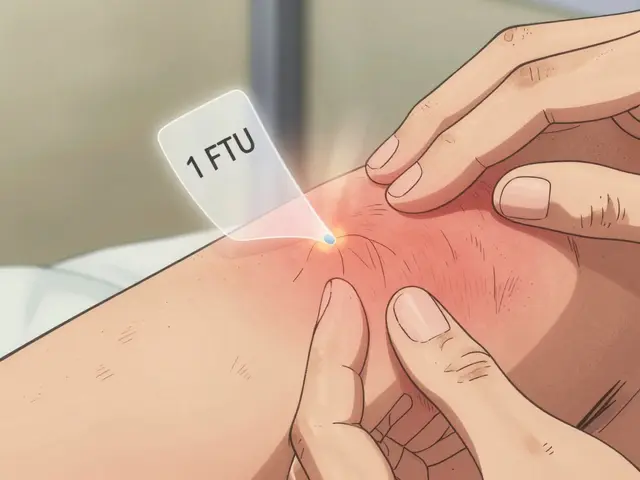
- Improper inhaler technique: If the medication doesn’t reach the lower airways, the attack won’t be aborted.
Understanding these risk factors helps patients and caregivers stay ahead of the curve.
Tips to Recognise Early Warning Signs
Catch an attack before it peaks. Look for these subtle cues:
- Increased need to cough, especially at night.
- Feeling tightness around the chest or throat.
- Worsening shortness of breath during routine activities.
- Whistling sound when exhaling (even if faint).
- Reduced peak flow readings (if you use a peak flow meter).
When any of these appear, reach for your rescue inhaler immediately and consider a short‑acting oral steroid if the attack doesn’t ease within 15‑20 minutes.
Frequently Asked Questions
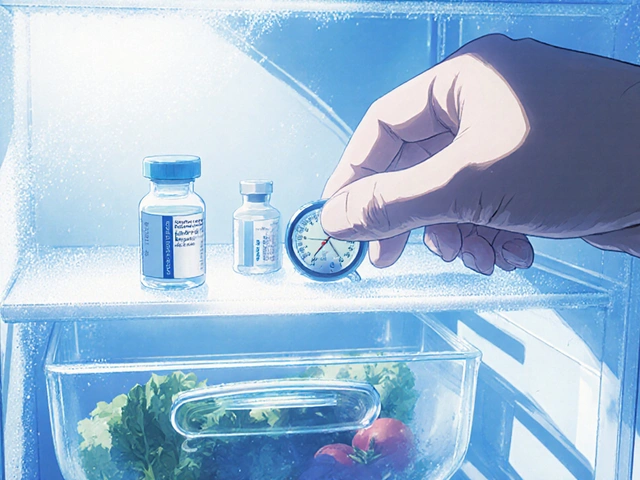
What is the difference between a rescue inhaler and a controller?
A rescue inhaler (short‑acting bronchodilator) works within minutes to relax the airway muscles during an attack. A controller (inhaled corticosteroid or a long‑acting bronchodilator) is taken daily to keep inflammation low and prevent attacks from happening.
Can I exercise if I have asthma?
Yes, most people can stay active. The key is to warm up slowly, use a rescue inhaler 10‑15 minutes before starting, and avoid extremely cold or polluted environments.
Why does my asthma get worse during a cold?
Viruses irritate the airway lining, increase mucus production, and boost inflammatory cytokines. This double‑hit-more swelling plus heightened sensitivity-makes attacks more likely.
Do I need to see a specialist if my attacks are frequent?
If you need your rescue inhaler more than twice a week, it’s time to see an allergist or pulmonologist. They can adjust your medication plan, test for specific allergens, and teach proper inhaler technique.
Can diet affect asthma attacks?
Some studies show that omega‑3 fatty acids, antioxidants, and a diet low in processed foods may lessen airway inflammation. However, dietary changes alone won’t replace prescribed medication.



Patrick Culliton
October 12, 2025 AT 03:36Everyone jumps on the allergen bandwagon, but the true trigger behind an asthma flare‑up is the hyperreactive airway smooth muscle contracting way too hard. When irritants hit the lungs, the muscles tighten, cutting airflow and sparking that dreaded wheeze. Add to that the inflammatory cascade releasing histamine and leukotrienes, and you’ve got a perfect storm. Bottom line: it’s not just pollen; it’s a cascade of physiological responses you can’t ignore.
Andrea Smith
October 16, 2025 AT 18:43I wholeheartedly concur with the physiological perspective you outlined, and I would like to emphasize that modern inhaled corticosteroids effectively dampen the inflammatory cascade you described. Moreover, patient education on trigger avoidance complements pharmacologic therapy, leading to improved control. It is essential that clinicians adopt a holistic approach, integrating both medication adherence and environmental modifications. By doing so, we empower individuals to anticipate and mitigate attacks before they become severe.
Gary O'Connor
October 21, 2025 AT 09:50yo, if ur dealing with asthma, just remember that stress can mess w/ your breathing even if you think it's just a cold. i’ve seen ppl get a tiny sniffle and suddenly they’re gaspin’ for air. always keep that rescue inhaler handy, cuz you never know when the next surprise will hit.
Justin Stanus
October 26, 2025 AT 00:56It’s terrifying to feel the world shrink as your chest tightens and you can’t draw a full breath. The panic that follows isn’t just in your head; the body’s stress response intensifies the bronchoconstriction, creating a vicious loop. That lingering sense of vulnerability can shadow daily life, making even simple tasks feel monumental. Recognizing that emotional intensity feeds the physical symptoms is the first step toward breaking the cycle.
Claire Mahony
October 30, 2025 AT 15:03While many attribute attacks solely to external allergens, it’s crucial to recognize the role of baseline airway hyperresponsiveness that often goes unchecked. Ignoring this intrinsic factor can lead to suboptimal treatment plans that focus only on avoidance. A thorough pulmonary function assessment should be standard practice before prescribing rescue medications.
Andrea Jacobsen
November 4, 2025 AT 06:10I completely agree with the need for comprehensive pulmonary testing; it provides a clear baseline from which we can gauge treatment efficacy. In addition, incorporating a personalized action plan ensures patients know precisely when to step up therapy. Collaborative care, involving both clinicians and patients, yields the best outcomes.
Andrew Irwin
November 8, 2025 AT 21:16It’s understandable that differing opinions on treatment emphasis can cause friction, yet both environmental control and physiological assessment are vital pieces of the puzzle. Striking a balance between the two respects individual experiences while maintaining evidence‑based practice. Ultimately, our shared goal is to reduce the frequency and severity of attacks for everyone.
Jen R
November 13, 2025 AT 12:23Honestly, the article could’ve saved a few paragraphs by just stating that inhaled corticosteroids are the cornerstone of long‑term control. Most of the extra detail about cytokine pathways feels like filler for the sake of sounding scientific. If you want a quick takeaway, stick to the basics: meds, trigger avoidance, and regular check‑ups.
Joseph Kloss
November 18, 2025 AT 03:30One might argue that an asthma attack is not merely a physiological event but a reminder of the body’s dialogue with the environment. When the airway narrows, it whispers that the external world has overstepped its bounds, demanding respect. This interplay of chemical mediators and neural feedback forms a microcosm of larger ecological balances. Observing the cascade can teach us humility about our perceived control over internal systems. Thus, managing asthma becomes both a medical and philosophical exercise.
Anna Cappelletti
November 22, 2025 AT 18:36Great insight on the body‑environment interaction; just a minor note: “overstepped” should be hyphenated when used as an adjective (“over‑stepped”). Your explanation elegantly ties the physiological response to a broader perspective, which can motivate patients to stay proactive. Keep up the balanced, uplifting tone-it's both informative and reassuring.
Dylan Mitchell
November 27, 2025 AT 09:43When the first breath feels like a thief in the night, stealing air with ruthless precision, the drama of an asthma attack unfolds in vivid detail. The bronchial tubes, normally gentle highways, suddenly contract like clenched fists, refusing to let oxygen pass. A cascade of inflammatory mediators erupts, each one a tiny villain launching its own assault on the already strained passages. Histamine, leukotrienes, and prostaglandins join forces, swelling the mucosal lining until it resembles a storm‑tossed sea. The patient, caught in this maelstrom, experiences a tightness that is not merely physical but profoundly psychological. The mind races, heart pounds, and tears of frustration may well accompany the wheeze, turning the episode into a theatrical performance of desperation. Yet, amidst the chaos, a rescue inhaler stands as the fleeting hero, delivering a bronchodilator that forces open the stubborn gates. Its swift action can transform the scene from a tragedy into a brief intermission, allowing the protagonist to breathe once more. Nevertheless, the underlying hyperresponsiveness remains, a lurking antagonist waiting for the next cue. Proper maintenance therapy, such as inhaled corticosteroids, acts as the seasoned director, gently guiding the production toward a calmer resolution. Education on trigger avoidance serves as the stage manager, ensuring that unexpected props do not sabotage the show. When patients internalize this script, they gain the power to anticipate and rewrite the narrative before the climax erupts. Moreover, regular monitoring of lung function provides a backstage pass, revealing subtle changes before they become catastrophic. In this way, the drama of asthma can be transformed from an uncontrollable catastrophe to a manageable performance. Remember, the body is both the actor and the audience; by treating it with respect, we can rewrite the ending. So, breathe deep, stay prepared, and let science be the spotlight that guides you through the darkness.
Elle Trent
December 2, 2025 AT 00:50Integrating pharmacodynamics with patient adherence metrics optimizes the therapeutic index.