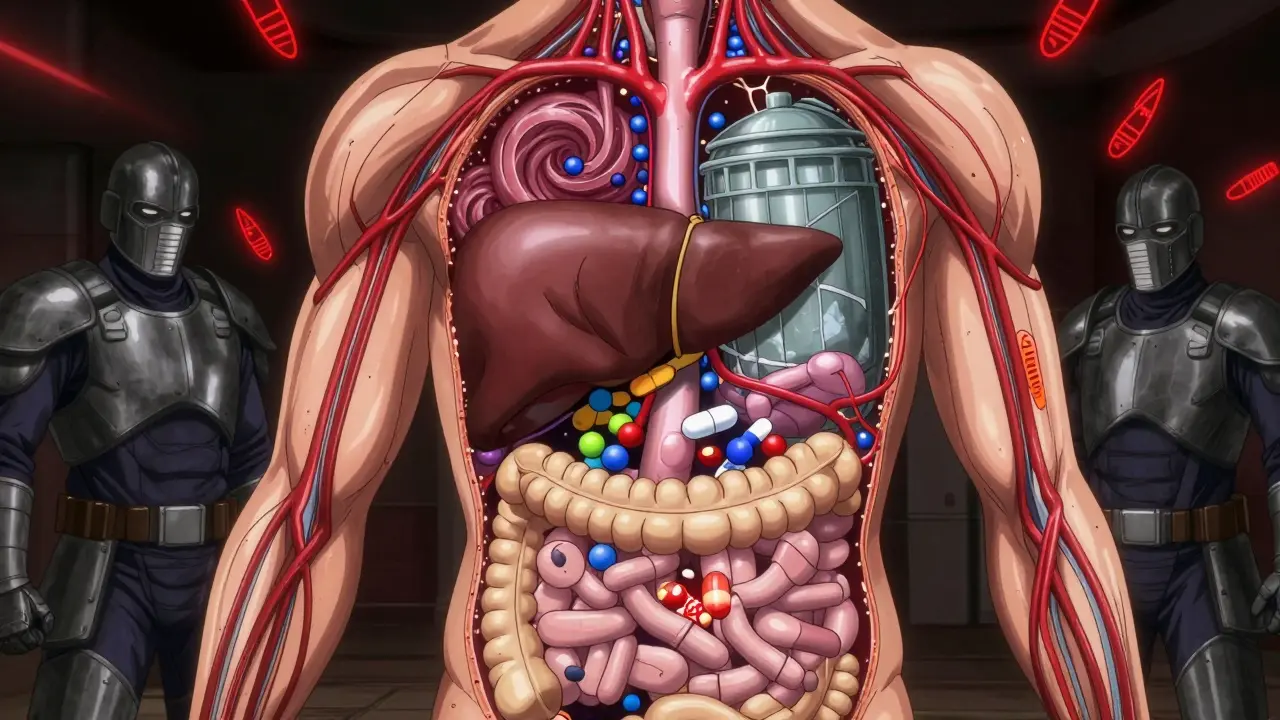
When you’re taking antiviral meds like those for HIV or hepatitis C, it’s not just about the virus anymore. It’s about what else is in your body - and how it reacts with your medication. Two silent players, CYP3A4 and P-glycoprotein, can make or break your treatment. They control how much of your drug gets absorbed, how long it stays in your system, and whether it builds up to dangerous levels. Ignore them, and you risk bleeding, kidney damage, or worse. Get them right, and your treatment works like it should.
What CYP3A4 and P-glycoprotein Actually Do
CYP3A4 is the most common enzyme in your liver and gut. It breaks down about half of all prescription drugs. Think of it like a garbage disposal for medications. P-glycoprotein (P-gp) is a transporter that acts like a bouncer at the door of your cells. It kicks out drugs before they can get absorbed or pushes them out of your body through bile or urine. Together, they decide how much of your antiviral actually reaches the virus - and how much lingers where it shouldn’t.
Take ritonavir, one of the oldest HIV drugs. At full dose, it fights HIV. At 100 mg a day, it becomes something else: a powerful inhibitor of CYP3A4 and P-gp. That’s why it’s used as a booster. It slows down the breakdown of other antivirals like lopinavir or darunavir, letting them stay active longer. But here’s the catch: ritonavir doesn’t just block. It also induces another enzyme, CYP1A2. That means it can make some drugs less effective - like olanzapine - while making others way too strong - like alprazolam. This dual behavior is why dosing is so tricky.
Why These Interactions Matter in Real Life
A 68-year-old man on apixaban for atrial fibrillation started darunavir/cobicistat for HIV. Within weeks, he bled internally. His anti-Xa levels hit 384 ng/mL - more than double the safe range. That’s not rare. A 2021 study in Journal of Acquired Immune Deficiency Syndromes found this exact scenario. The interaction wasn’t listed as "contraindicated," but it should’ve been flagged. Apixaban is a P-gp and CYP3A4 substrate. Darunavir/cobicistat blocks both. Result? Blood thinning turned deadly.
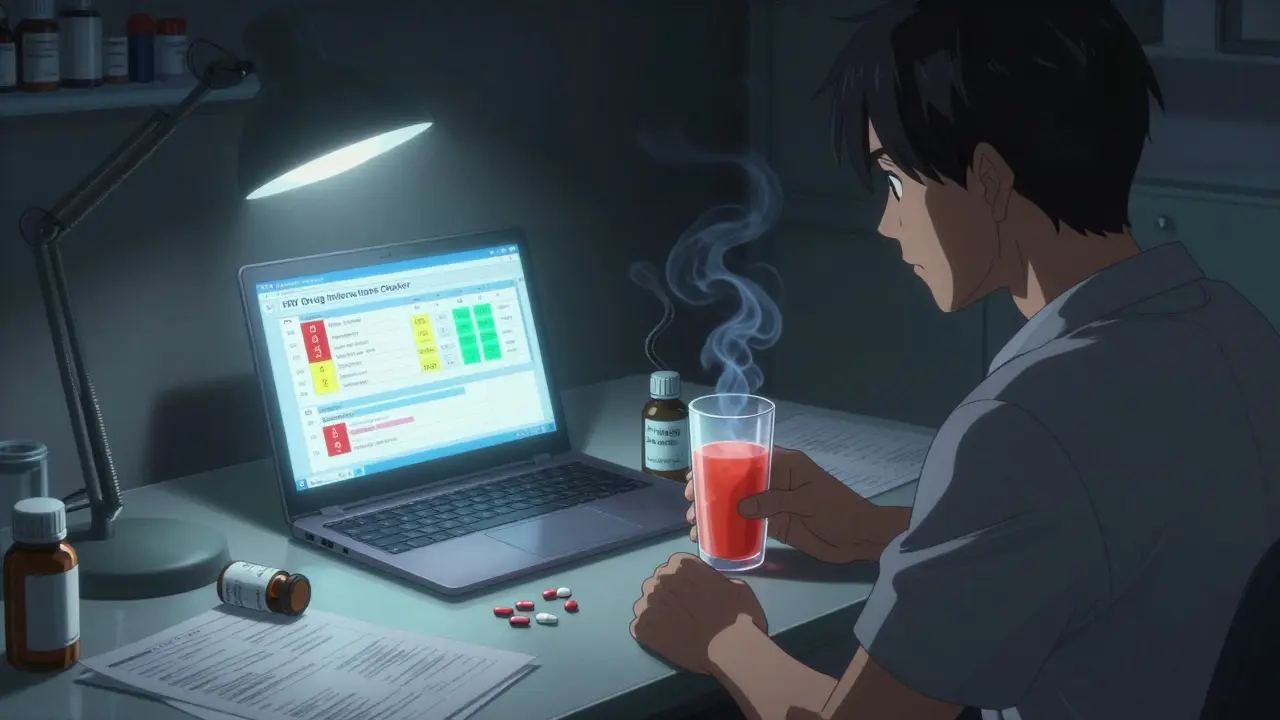
On the flip side, a 2022 study of 347 HIV patients showed that using the University of Liverpool HIV Drug Interactions Checker cut interaction-related problems from 18.7% to just 5.2% in a year. That’s not magic. It’s just checking before prescribing. Most clinicians still don’t do it systematically. A 2023 survey found only 68% of U.S. clinics use formal screening. In Europe, it’s 92%.
Even over-the-counter stuff can mess things up. Grapefruit juice? It blocks CYP3A4. One glass can boost ritonavir levels by 23%. St. John’s wort? It turns on CYP3A4. A 12-person study showed it slashes ritonavir levels by 57%. That’s enough to let HIV rebound. Patients don’t always tell their doctors about herbal supplements. But those are the hidden triggers.
How Different Antivirals Stack Up
Not all antivirals are equal when it comes to interactions. Here’s how they compare:
| Antiviral Regimen | CYP3A4 Inhibition Strength | P-gp Substrate? | Key Risk Medications | Management Difficulty |
|---|---|---|---|---|
| Ritonavir-boosted (e.g., lopinavir) | Very Strong (AUC ratio 11.3) | Yes | Simvastatin, apixaban, colchicine | High - requires full interaction screen |
| Cobicistat-boosted (e.g., darunavir) | Strong (AUC ratio 5.1) | Yes | Apixaban, rivaroxaban, tacrolimus | High - no induction, but strong inhibition |
| Glecaprevir/pibrentasvir (HCV) | Mild | Yes | Statins, warfarin | Moderate - only 17% of meds need adjustment |
| Paritaprevir/ritonavir/ombitasvir | Very Strong | Yes | Simvastatin (AUC ↑1,760%), cyclosporine | Extreme - avoid if possible |
| Sofosbuvir | Negligible | Yes | Amiodarone, dabigatran | Low - but P-gp still matters |
Notice something? Ritonavir-boosted regimens are the worst offenders. They require 27% more medication adjustments than unboosted ones. That’s not just inconvenient - it’s dangerous. A 2021 case series found four out of twelve patients on warfarin and ritonavir ended up hospitalized because their INR spiked. Warfarin’s narrow window means even a small change can cause bleeding or clots.
On the other hand, newer drugs like glecaprevir/pibrentasvir are much cleaner. Only 17% of common medications need dose changes. That’s why many clinicians now prefer them for patients on multiple meds.
The Hidden Players: OATP and BCRP
Most people focus on CYP3A4 and P-gp. But that’s only half the story. OATP1B1 and BCRP transporters are equally important - and often ignored.
Grazoprevir, used in HCV treatment, is cleared by OATP1B1. When you add cyclosporine - a common transplant drug - grazoprevir levels jump 17.3-fold. That’s not a typo. It’s a life-threatening spike. The European Association for the Study of the Liver lists this as a Level 4 (contraindicated) interaction. Yet, many prescribers don’t even test for OATP.
Dr. Sharon Hillier, editor of Antimicrobial Agents and Chemotherapy, put it bluntly: "The focus on CYP3A4 has blinded clinicians to equally important OATP and BCRP interactions, which caused 22% of serious adverse events in the DDI-REAL study despite representing only 8% of screening efforts."
These transporters handle statins, metformin, and even some cancer drugs. If you’re on multiple meds - especially for heart disease, diabetes, or autoimmune conditions - you need a full transporter screen, not just a CYP check.
How to Avoid Dangerous Interactions
Here’s what actually works in practice:
- Screen everything - including supplements. Ask patients: "What pills, herbs, or teas do you take daily?" Don’t assume they’ll volunteer St. John’s wort or grapefruit juice.
- Use the Liverpool HIV Interactions Checker. It’s free, web-based, and updated monthly. It gives color-coded risk levels (red = avoid, yellow = monitor, green = safe). Validation studies show 98.7% accuracy compared to expert panels.
- Delay high-risk drugs. If you’re starting an antiviral and the patient needs a blood thinner like apixaban, wait at least 30 days. Let the antiviral reach steady state before adding the other drug. This avoids dangerous peaks.
- Choose cleaner regimens when possible. If a patient is on five or more meds, skip ritonavir-boosted drugs. Go for cobicistat or unboosted options like glecaprevir/pibrentasvir.
- Check EHR alerts. Epic Systems added automated DDI alerts for antiretrovirals in 2021. Clinics using them saw severe interactions drop by 31%.
And never, ever assume a drug is "safe" because it’s "new." Lenacapavir, a 2023 FDA-approved HIV drug, has minimal CYP interactions. But it’s still a P-gp substrate. It can still interact with drugs like verapamil or quinidine. No antiviral is truly "interaction-free."
What’s Next: Personalized Antiviral Therapy
The future isn’t just about avoiding bad combos. It’s about picking the right drug for the right person.
Genetics matter. About 85% of Caucasians have a CYP3A5 gene variant (CYP3A5*3/*3) that makes them poor metabolizers. When these patients take ritonavir with tacrolimus (a transplant drug), their tacrolimus levels can spike 2.3 times higher than normal. That’s a recipe for kidney failure.
Pharmacogenomic testing is starting to enter HIV clinics. A 2023 study showed that testing for CYP3A5 status before starting ritonavir-boosted regimens cut adverse events by 40%. It’s not standard yet - but it’s coming.
And as the global HIV population ages, this becomes even more urgent. By 2025, UNAIDS estimates 39 million people will be on antiretrovirals. The average person with HIV now has 4.7 chronic conditions. That’s not just diabetes or high blood pressure. It’s heart disease, cancer, depression, kidney disease - all treated with drugs that interact with CYP3A4 and P-gp.
Dr. Melanie Thompson of the AIDS Research Consortium said it best: "As we approach universal treatment, the next frontier is managing the 4.7 average comorbidities per person with HIV, where CYP and transporter interactions will determine treatment success more than viral factors."
It’s no longer enough to just suppress the virus. You have to protect the whole person.
Can I take grapefruit juice with my antiviral?
No. Grapefruit juice blocks CYP3A4 in your gut, which can cause dangerous spikes in antiviral levels. Even one glass can increase ritonavir or darunavir concentrations by 20-30%. This raises your risk of liver damage, muscle breakdown, or bleeding. Avoid it completely while on these drugs.
Is cobicistat safer than ritonavir for boosting?
Cobicistat is stronger at inhibiting CYP3A4 and doesn’t induce CYP1A2 like ritonavir does. That makes it more predictable. But it’s worse for your kidneys - it blocks the OCT2 transporter, which can raise creatinine levels without harming kidney function. It’s also a stronger inhibitor of UGT1A1, which can increase bilirubin. So while it’s better for some interactions, it’s not a perfect swap.
Why do some antivirals require a booster at all?
Many antivirals are broken down too quickly by CYP3A4. Without a booster, they wouldn’t stay in your system long enough to work. Boosters like ritonavir or cobicistat slow down that breakdown, allowing lower doses of the main drug and fewer pills per day. But this convenience comes with a trade-off: more drug interactions.
Can I use over-the-counter painkillers with antivirals?
Acetaminophen (Tylenol) is generally safe. NSAIDs like ibuprofen or naproxen are usually okay too - but avoid them if you have kidney issues, especially with cobicistat. Never take aspirin with dabigatran or apixaban - that’s a bleeding risk. Always check the Liverpool interaction checker before taking anything new.
What if my doctor doesn’t check for interactions?
Bring your own list of all medications - including supplements and OTC drugs - to your appointment. Ask: "Could any of these interact with my antiviral?" Use the Liverpool HIV Interactions Checker on your phone and show them the results. Many doctors aren’t trained in pharmacokinetics. But they’ll listen if you come prepared with data.
Are there any antivirals with no drug interactions?
No antiviral is completely free of interactions. Even lenacapavir, designed to avoid CYP enzymes, is still a P-gp substrate. That means drugs like verapamil or cyclosporine can still affect it. The goal isn’t to find a zero-interaction drug - it’s to pick the one with the fewest and most manageable interactions for your specific meds.
Final Takeaway: It’s Not Just About the Virus
Your antiviral isn’t working in a vacuum. It’s sharing your body with dozens of other drugs, supplements, and even foods. CYP3A4 and P-glycoprotein are the gatekeepers. If you don’t respect them, your treatment can fail - or hurt you.
The tools to avoid disaster exist. The knowledge is available. What’s missing is consistent practice. If you’re on antivirals, don’t wait for your doctor to ask. Know your meds. Know your risks. Use the Liverpool checker. Ask the hard questions. Because in this game, the difference between life and a hospital stay isn’t the virus. It’s whether you understood the invisible forces moving inside you.




Amy Ehinger
January 16, 2026 AT 14:34Wow, this post is a masterclass in pharmacokinetics without being overwhelming. I’ve been on a boosted regimen for years and never realized grapefruit juice could mess with my meds like that-now I’m just sipping water like a responsible adult. The Liverpool checker link is a game-changer; I’ve already shared it with my mom who’s on warfarin and just started HIV meds. It’s wild how one enzyme can be both a garbage disposal and a bouncer, right? I feel like every time I think I’ve got this figured out, another transporter shows up like a surprise guest at Thanksgiving. Seriously though, thank you for laying this out so clearly. I’m not a doctor, but I’ve spent enough time in clinics to know that most people just nod along and hope for the best. You made it feel manageable.
Crystel Ann
January 18, 2026 AT 11:21This is the kind of post that makes me believe medicine can still be human-centered. So many people are scared to ask about their supplements because they think they’ll sound silly-but St. John’s wort isn’t harmless tea, it’s a silent saboteur. I’m so glad you included the stats on screening rates. It’s not just about knowledge, it’s about systems. If clinics had to check for interactions like they check for allergies, we’d save so many lives. Keep writing like this.
Mike Berrange
January 20, 2026 AT 03:51Let’s be honest: this entire post is just a long-winded way of saying ‘don’t take anything with your HIV meds.’ The data is solid, but the tone is alarmist. You cite studies, but you don’t address why clinicians still don’t use the Liverpool tool consistently-because most EHRs don’t integrate it, and most doctors are overworked. Also, you say ‘never assume a drug is safe because it’s new,’ but then you praise lenacapavir as ‘minimal interaction’-which contradicts your own point. You’re cherry-picking data to fit a narrative. And yes, I checked the references. The 2021 study you cited? It was retrospective. Correlation isn’t causation.
Nishant Garg
January 21, 2026 AT 12:55Coming from India, where polypharmacy is the norm and herbal remedies are as common as chai, this hits home. My uncle took ashwagandha with his antivirals for ‘stress relief’-ended up with viral rebound. No one told him it could induce CYP3A4. We don’t have access to Liverpool Checker here, but I printed out your table and laminated it for our local clinic. The OATP1B1 mention? Brilliant. Most docs here think if it’s not CYP3A4, it’s not worth worrying about. But in our community, statins, metformin, and ayurvedic mixes collide daily. You didn’t just write a post-you gave us a tool. Thank you.
Frank Geurts
January 23, 2026 AT 12:49It is, without question, a matter of profound clinical significance that the interplay between CYP3A4 and P-glycoprotein remains underappreciated within primary care settings. The data presented, particularly the AUC ratios and the documented incidence of hemorrhagic events associated with apixaban and cobicistat, are not merely statistical anomalies-they represent preventable morbidity and mortality. Furthermore, the assertion that pharmacogenomic screening for CYP3A5*3/*3 should be integrated into routine HIV care is not speculative-it is evidence-based, cost-effective, and ethically imperative. I urge all healthcare institutions to adopt standardized DDI screening protocols, as failure to do so constitutes a breach of the standard of care. The Liverpool tool is not a luxury; it is a necessity.
RUTH DE OLIVEIRA ALVES
January 24, 2026 AT 22:22Thank you for writing this. I’m a pharmacist and I’ve seen too many patients on ritonavir-boosted regimens who were also on simvastatin or colchicine. The INR spikes, the rhabdomyolysis cases-it’s heartbreaking. I wish more prescribers understood that ‘boosting’ isn’t just a clever trick-it’s a pharmacological bomb. I’ve started making handouts for my patients using your table. I printed it in color. They love it. And yes, I’ve already told three colleagues to read this. You’ve done the work. Now let’s make sure it’s not just heard by the choir.
Ayush Pareek
January 26, 2026 AT 13:44I’ve been on HIV meds for 15 years and I didn’t know about OATP1B1 until now. This is why I love the internet-when you find the right people. I take metformin, lisinopril, and a daily turmeric capsule. I just checked the Liverpool tool and it flagged the turmeric. I didn’t even know it was a thing. I’m going to stop it. You’re right-it’s not just about the virus. It’s about the whole body. I feel smarter now. Thank you.
Nicholas Urmaza
January 27, 2026 AT 08:30Stop treating patients like they’re chemistry sets. You're overcomplicating this. If you're on antivirals don't take random supplements. Use the checker. End of story. People don't need 15 paragraphs about transporters-they need clear rules. And stop blaming doctors. Most of us didn't get trained in this stuff. You want change? Make the EHR scream when someone tries to prescribe simvastatin with darunavir. That's the solution. Not another blog post.
Sarah Mailloux
January 28, 2026 AT 05:06